CELL:研究人员分化出房室特异性心脏组织,用于疾病建模
2019-01-30 海北 MedSci原创
使用源自人多能干细胞的心肌细胞的组织工程有望彻底改变药物发现现状,但科学家们需要先克服与心室特异性和平台多功能性相关的限制。
使用源自人多能干细胞的心肌细胞的组织工程有望彻底改变药物发现现状,但科学家们需要先克服与心室特异性和平台多功能性相关的限制。
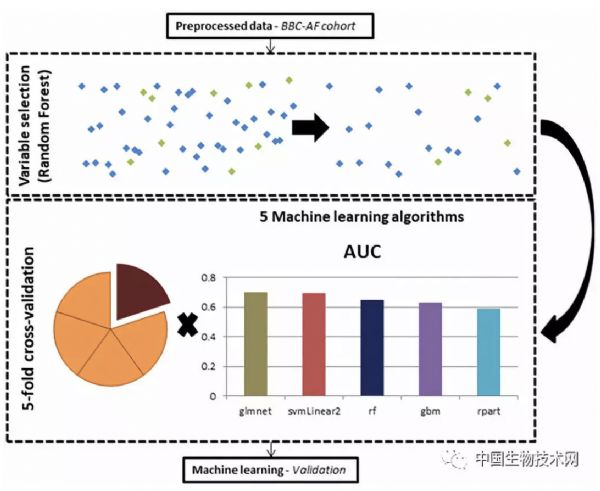
最近,研究人员报导了一种可扩展的组织培养平台,该平台是细胞源不可知的,并且能够在电起搏下进行药物测试。该塑料平台能够在线无创记录被动张力,主动力,收缩动力学和钙离子瞬变,以及动作电位和传导速度的终点评估。
通过将定向细胞分化与电场调节相结合,研究人员设计了具有腔室特异性药物反应和基因表达的电生理学上不同的心房和心室组织。
这是研究人员首次报道的包含不同心房和心室末端的异极心脏组织的工程,并且证明了它们对5-羟色胺和雷诺嗪的空间特异性反应。独特的是,8个月的电子调节使研究人员能够从患者细胞开始模拟多基因左心室肥大。
原始出处:
Zhao Y et al. A Platform for Generation of Chamber-Specific Cardiac Tissues and Disease Modeling. CELL, 2019; doi: 10.1016/j.cell.2018.11.042.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#研究人员#
30
#Cell#
37
#特异性#
41
#CEL#
36
嗯新思路
0
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
65
学习了长知识
58
学习了新知识
68
学习了长知识
65
学习了新知识
29