JACC:术中低血压增加死亡率?维持较高血压可能并不能减少不良预后!
2021-10-28 MedSci原创 MedSci原创
这些发现并不支持普遍以较高的术中血压为目标来减少术后并发症。
主要不良心血管事件(MACE)和心肌损伤是非心脏手术后发病和死亡的主要原因,30天的死亡率有三分之一可能是由心肌损伤引起的。已发现术中低血压与术后心血管疾病和全因死亡率密切相关。
然而,针对较高的术中血压(BPs)是否能改善术后结果,即术中低血压是否是疾病的标志或媒介,目前仍不清楚。特别是,目前还没有研究对心血管高危人群--术后并发症风险最高、可能从避免低血压发作中获益最大的患者--在重大非心脏手术中针对较高术中血压的单独效果进行研究。
近期,来自瑞士圣加仑州立医院的专家开展了相关研究,旨在探讨较高的术中平均动脉血压(MAP)是否能降低术后MACE的发生率,结果发表在JACC杂志上。
这项单中心随机对照试验将接受重大非心脏手术的心血管风险成人患者分配到术中MAP目标值≥60mmHg(对照)或≥75mmHg(MAP≥75)。主要结果是术后第0-3天的急性心肌损伤和/或30天的MACE/急性肾损伤(AKI)(急性冠状动脉综合征、充血性心力衰竭、冠状动脉血运重建、中风、AKI和全因死亡率)。次要结果是1年的MACE。
总共有458名患者接受了随机治疗(意向治疗人群:451人)。与MAP<65mmHg相比,MAP≥75组的累计术中时间明显缩短(中位数9分钟vs 23分钟)。同时,MAP≥75的主要结果发生率为48%,对照组为52%(风险差异为-4.2%;95%CI:-13%至+5%),主要因素是AKI(发生率为44%)。15%(MAP≥75)和19%(对照组)的患者发生急性心肌损伤。MAP≥75的次要结果发生率为17%,对照组为15%(风险差异+2.7;95%CI:-4%至+9.5%)。
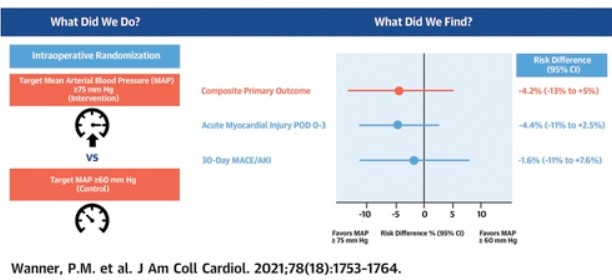
尽管术中低血压有重要的减少,但在主要的非心脏手术中以较高的术中血压为目标,与急性心肌损伤或30天主要不良心血管事件/急性肾损伤的发生率没有显著差异。
综上,这些发现并不支持普遍以较高的术中血压为目标来减少术后并发症。
参考文献:
Targeting Higher Intraoperative Blood Pressures Does Not Reduce Adverse Cardiovascular Events Following Noncardiac Surgery. J Am Coll Cardiol. 2021 Nov, 78 (18) 1753–1764
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
26
#ACC#
16
#不良预后#
39
#低血压#
50
#术中低血压#
32