Cell Death Differ:上皮和内皮细胞衍生的外泌体调节肺泡巨噬细胞的免疫平衡并影响多种肺部疾病
2021-03-26 xiaozeng MedSci原创
肺泡巨噬细胞(AMs)能够维持气道的免疫平衡,其紊乱可导致各种肺部疾病,包括急性肺损伤/急性呼吸窘迫综合征(ALI/ARDS)、肺纤维化(PF)、哮喘和慢性阻塞性肺病(COPD)。
肺泡巨噬细胞(AMs)能够维持气道的免疫平衡,其紊乱可导致各种肺部疾病,包括急性肺损伤/急性呼吸窘迫综合征(ALI/ARDS)、肺纤维化(PF)、哮喘和慢性阻塞性肺病(COPD)。
ALI/ARDS涉及单核细胞或中性粒细胞的过度募集,其能够破坏血管内皮屏障并引发血氧交换的障碍。PF是由肺上皮细胞的长期慢性损伤(如长期吸烟或吸毒)所引起的。AMs具有多种表型,其参与炎症反应,调节组织重塑和抗纤维化过程。然而,目前对与肺微环境中AMs调节免疫平衡的分子机制还知之甚少。
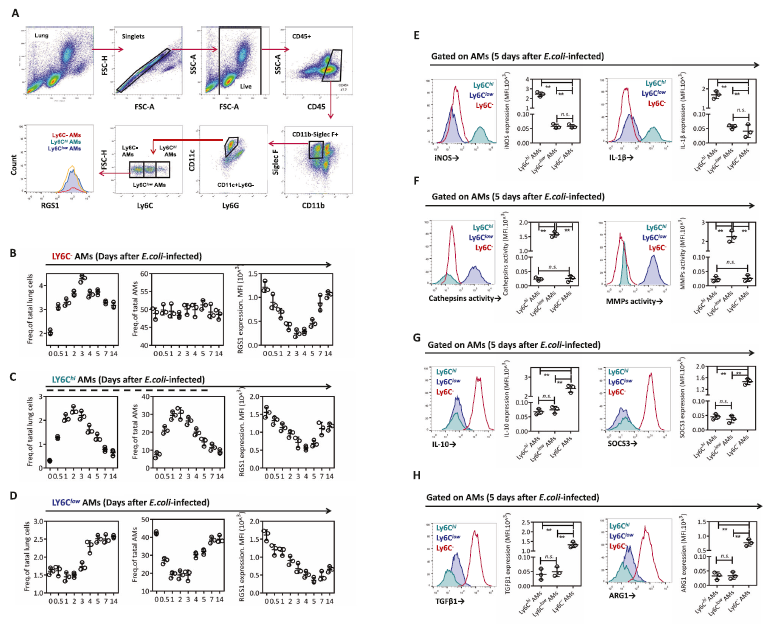
在该研究中,研究人员证实,RGS1能够通过PLC-IP3R信号依赖性细胞内Ca2+的响应调节AM细胞亚群的免疫表型,这些表型包括促炎和抗炎、损伤和修复以及促纤维化和抗纤维化的相关表型。
基于Ly6C表达的AMs的ALI/ARDS表型差异
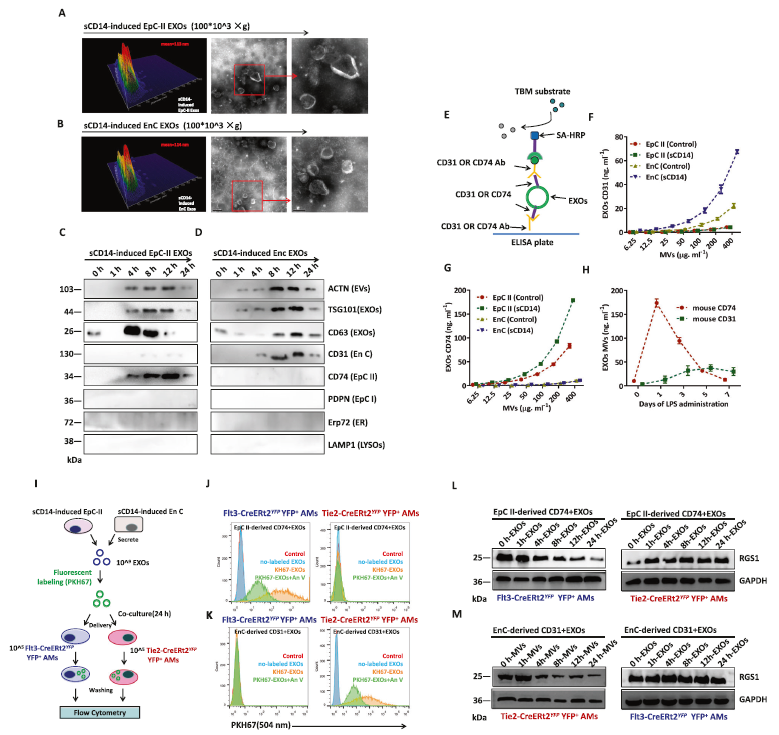
研究人员发现,Flt3+AM和Tie2+AM具有不同的免疫特性,且细胞中RGS1的表达被包含miR-223和miR-27b-3p的外泌体(EXO)所靶向,这些外泌体来自血管内皮细胞(EnCs)和II型肺泡上皮细胞(EpCs-II)。
EpCs-II和EnCs分泌的EXOs对Flt3+和Tie2+ AMs中RGS1表达的影响
进一步的研究显示,AMs的失衡与ALI/ARDS和PF中EnCs和EpCs-II衍生的CD31+和CD74+ EXO外泌体的分泌缺乏相关。而用EXOs治疗可以显著改善内毒素(endotoxin)诱导的ALI/ARDS和博来霉素(bleomycin)诱导的PF。
总而言之,该研究结果揭示,EnC和EpC-II衍生的EXO能够调节AM的免疫平衡,其或可成为潜在的治疗药物。
原始出处:
Feng, Z., Zhou, J., Liu, Y. et al. Epithelium- and endothelium-derived exosomes regulate the alveolar macrophages by targeting RGS1 mediated calcium signaling-dependent immune response. Cell Death Differ (22 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#肺泡巨噬细胞#
27
#Differ#
33
#CEL#
30
#Cell#
21
#Death#
31
#肺部疾病#
27