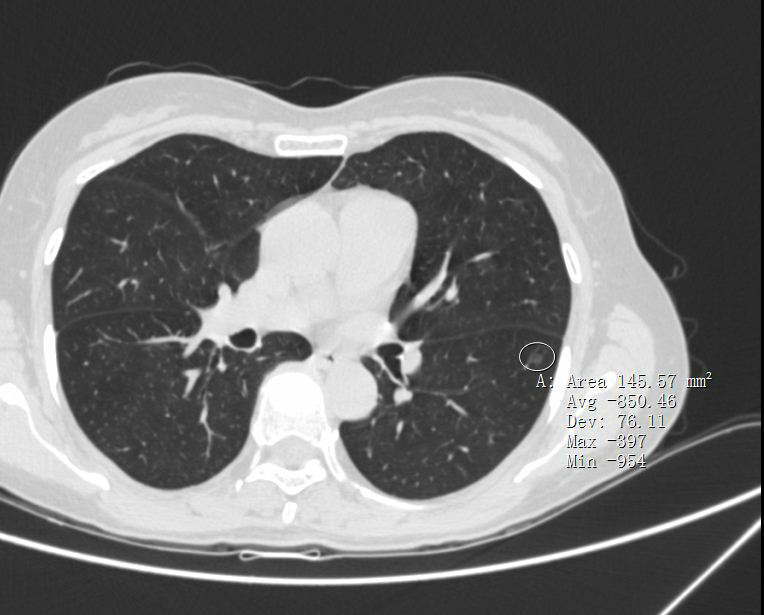
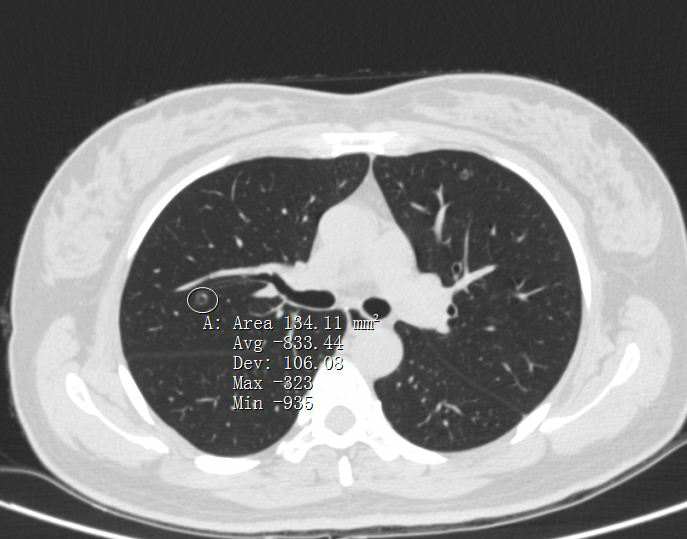
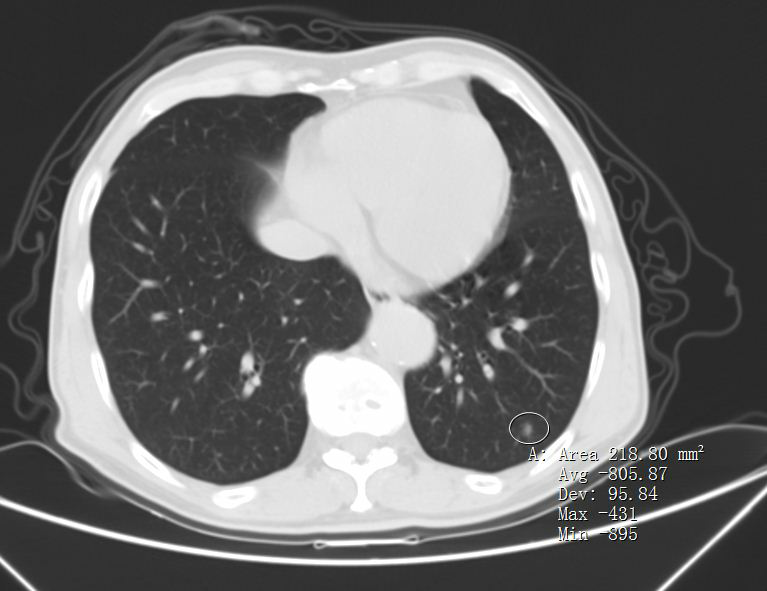
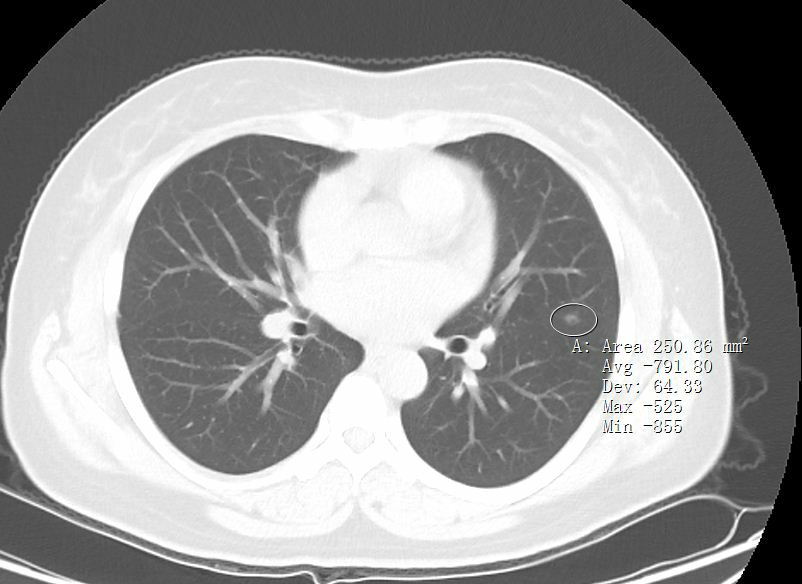
早期肺癌之原位癌AIS
2021-05-27 叶波 网络
原位癌(Adenocarcinoma in situ, AIS),是从正常组织转化为肿瘤细胞发展的第一个阶段。它的特性和影像特征,处理原则与浸润性癌有显著区别。
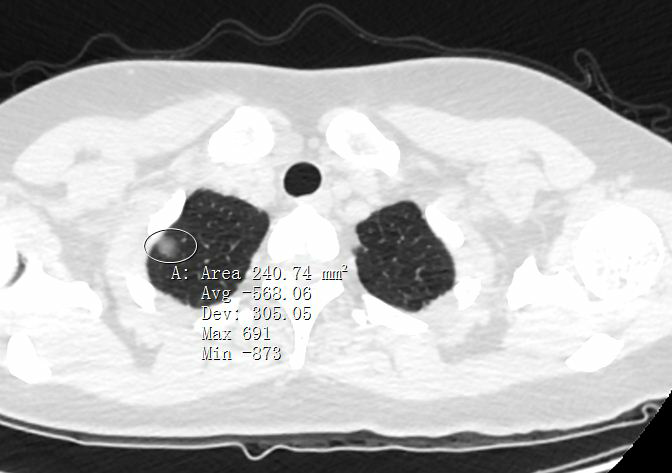
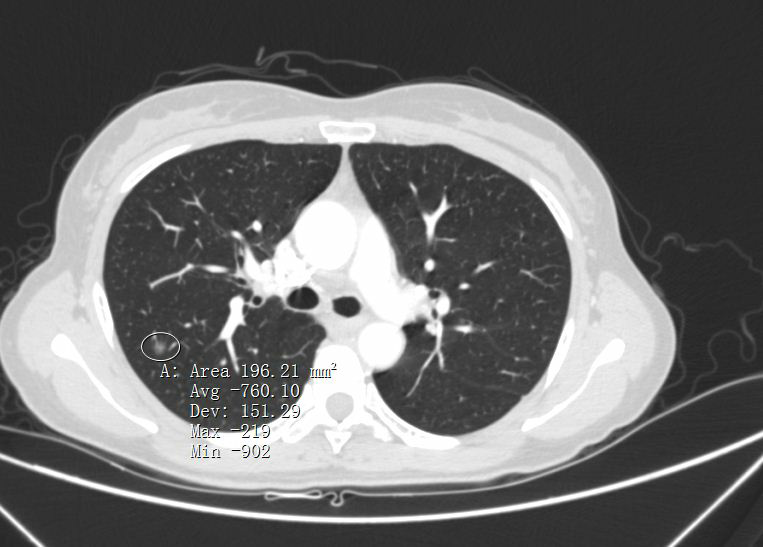
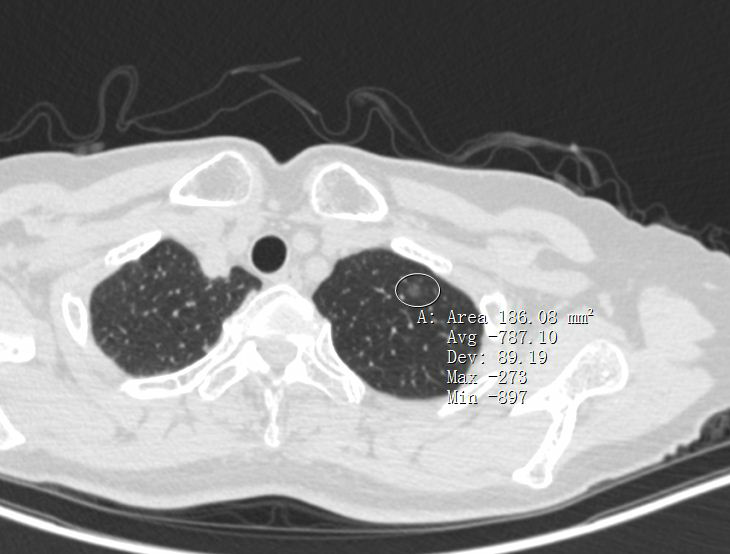
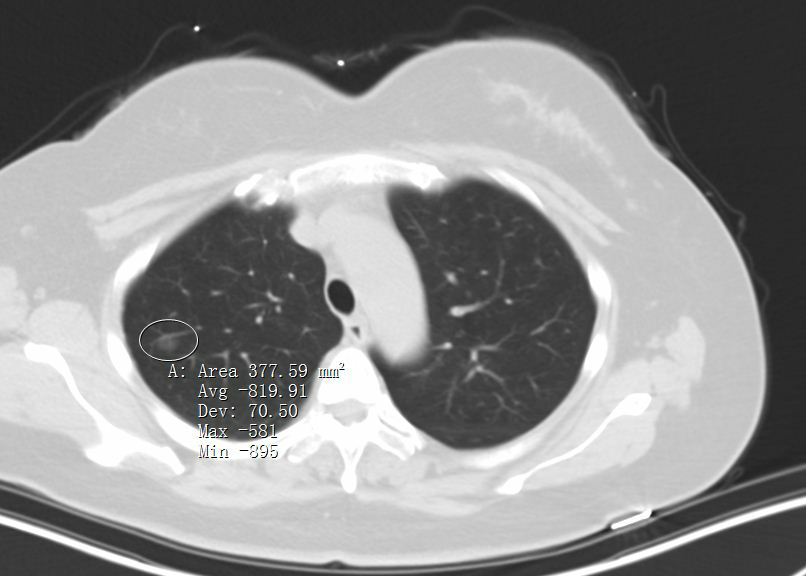
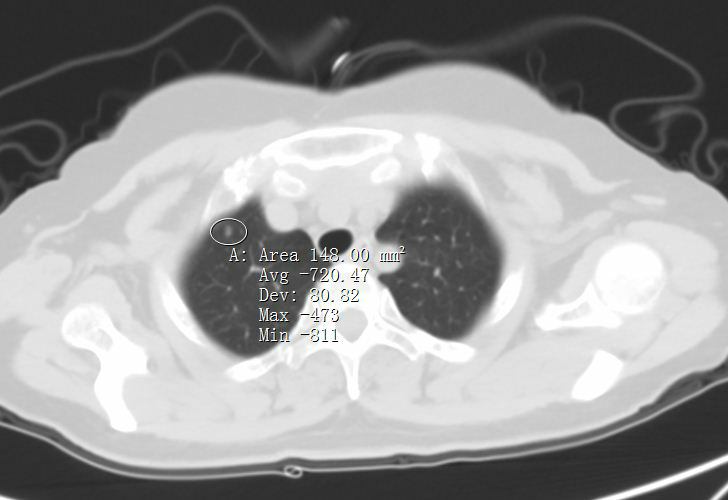
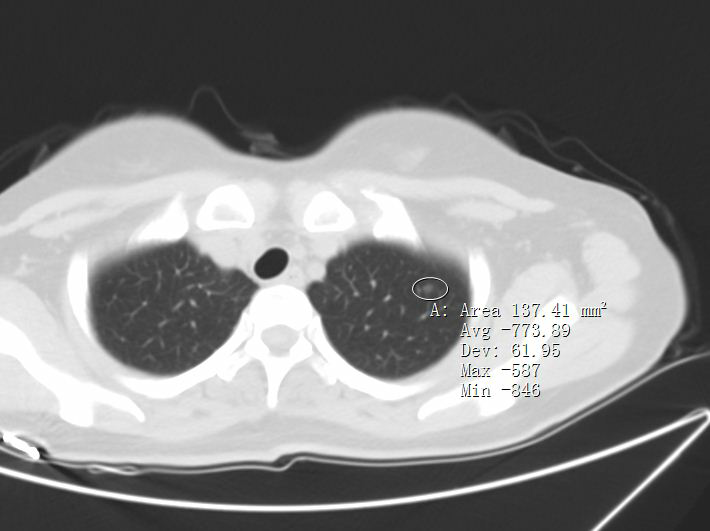
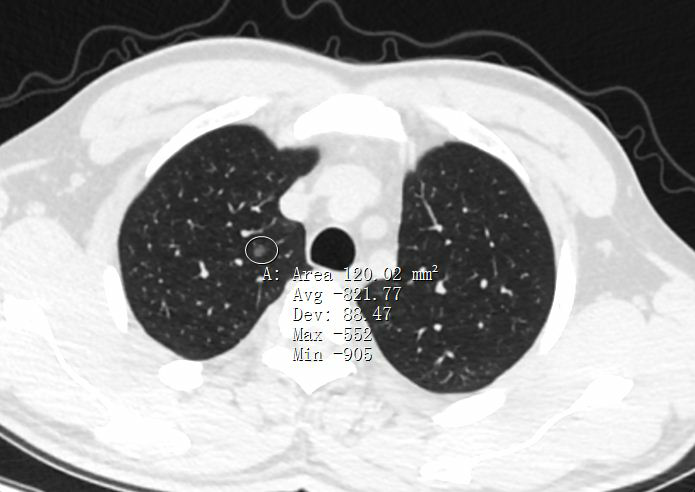
原位癌AIS的主要特性如下: 生长极为缓慢,大部分保持稳定10年以上。 不突破基底膜,意味着肿瘤局限于上皮层内,没有血管和淋巴管进入,因此不会发生远处和淋巴结转移。 切除后不会复发,不影响生存期。 以下均为近年来经我手术确诊的原位癌患者术前影像: 影像特征:多为<1cm的毛玻璃影,密度较低,可有毛刺、空泡,血管通过等高危特征,一般即使有血管通过,也无血管弯曲,也可无明显高危特征,但在随访过程中无明显变化。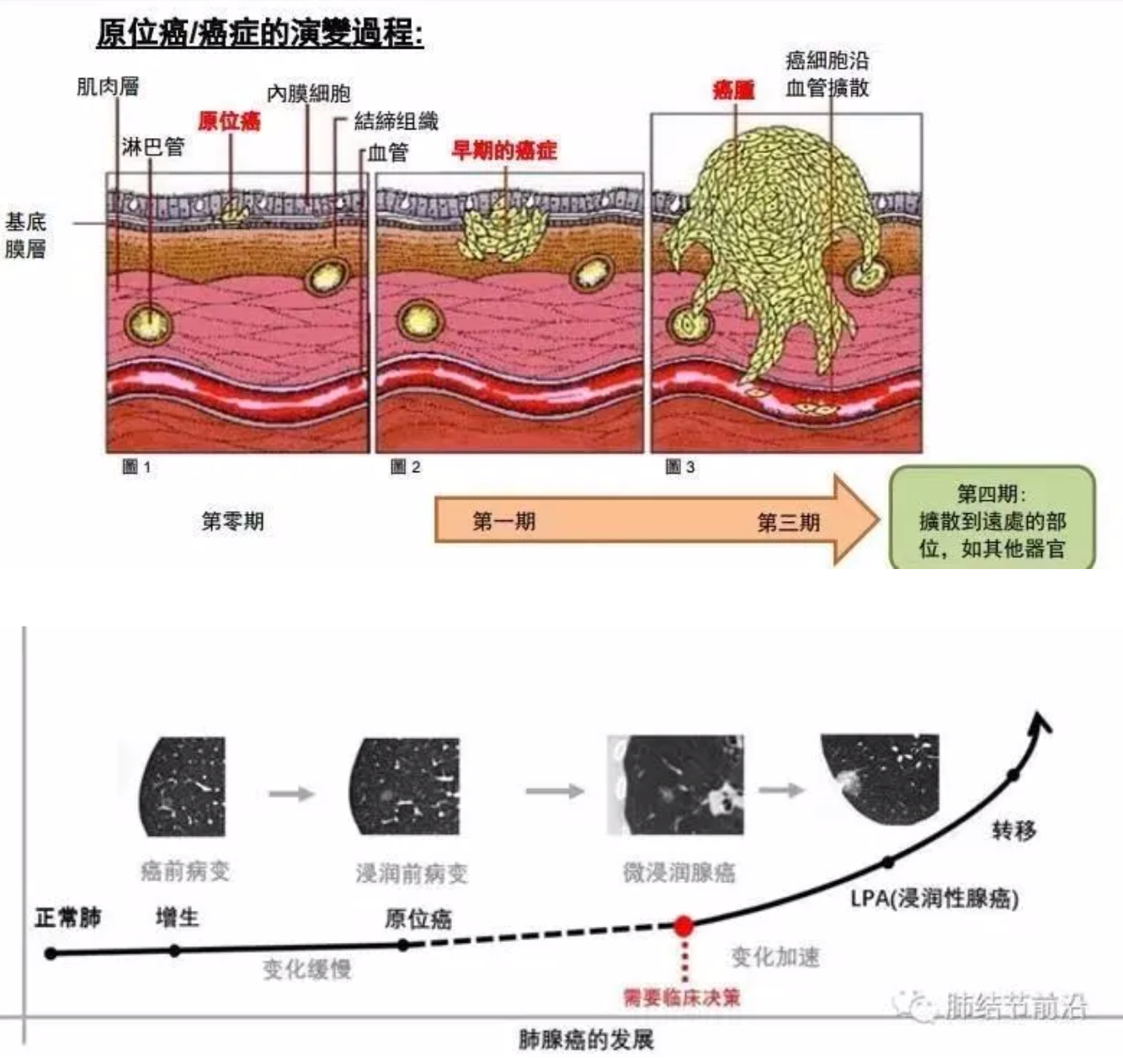
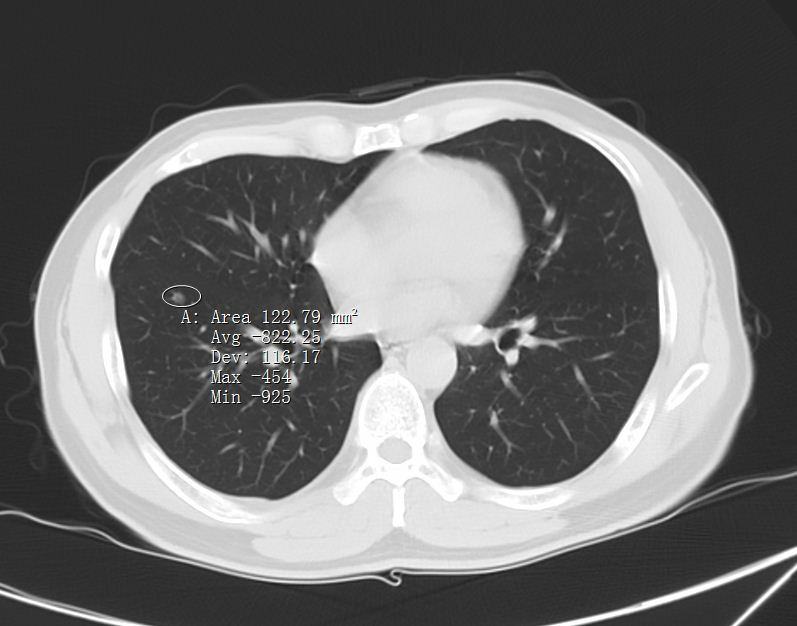
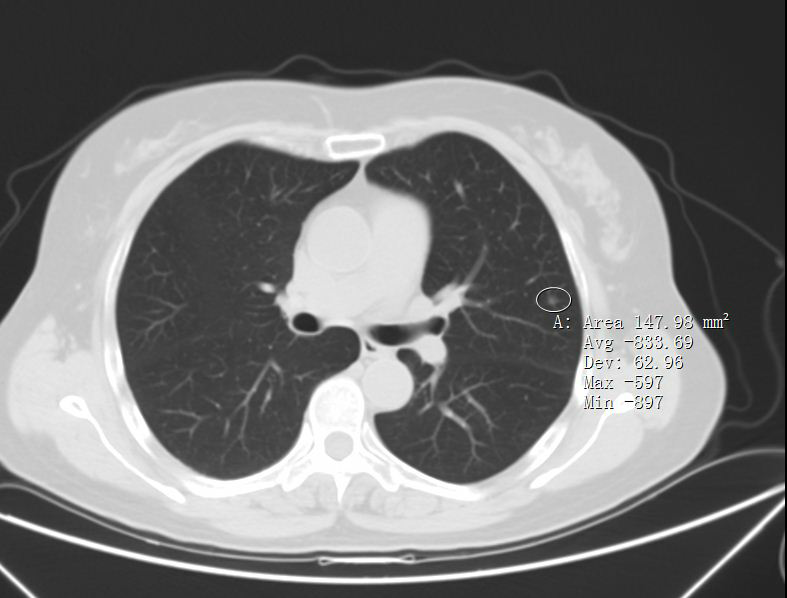
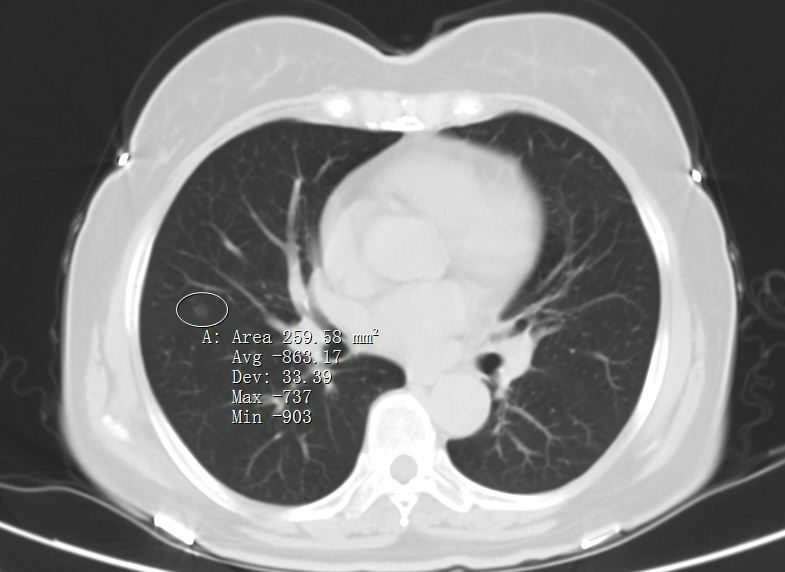
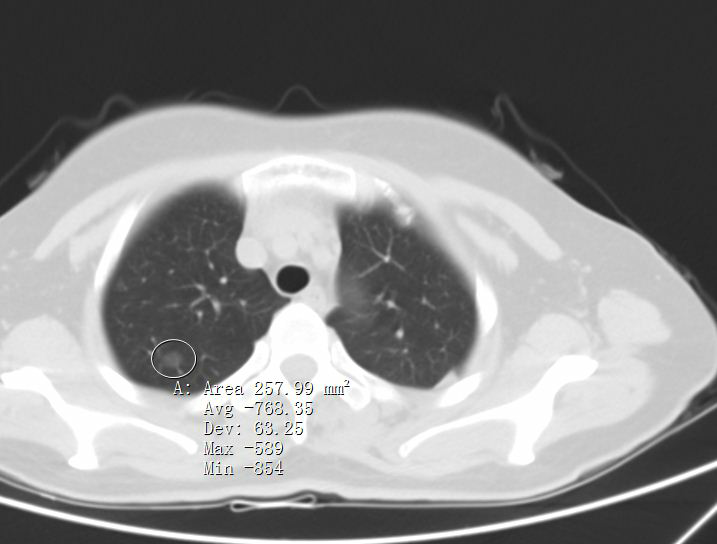

AIS的处理原则:由于原位癌生长缓慢,不会转移,此阶段对于身体没有危险性,2021年WHO已将原位癌剔除肺癌范畴,跟不典型增生一起,被认为是癌前病变,因此可以不手术切除,一般根据结节大小,建议6-12个月复查胸部CT随访。随访过程中,如发现结节变大,或密度增加等,提示有生长性,则再手术也来得及。如果患者心理压力比较大,或者结节>8mm,有较多高危特征,也可直接胸腔镜手术切除。需要注意的是,原位癌AIS切除后即治愈,不会复发,不需要术后辅助治疗。可以说,切除后就是正常人。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#AIS#
35
#原位癌#
27
#早期肺癌#
45