J Thromb Haemost:使用新型抗血栓药物治疗COVID-19的疗效分析
2021-09-23 MedSci原创 MedSci原创
这些新型抗血栓药物具有多效抗炎和抗病毒作用,可能有助于降低病毒载量或纤维化,并改善患者氧合。正在进行的RCT的结果将阐明它们在COVID-19患者治疗中的实际效用。
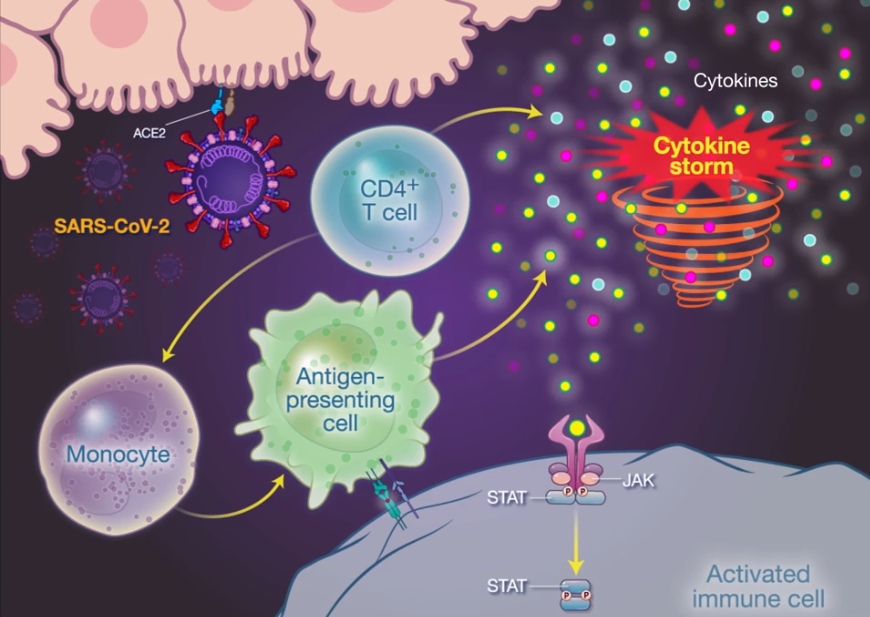
2019冠状病毒病(COVID-19)与宏观和微观血栓形成相关,这些血栓由内皮细胞活化、凝血病和不受控制的炎症反应所引发。数十项针对COVID-19患者的随机对照试验(RCT)正在评估常规抗血栓药物,但几项研究的初步结果并未发现益处。

近日,血栓和凝血疾病权威杂志Journal of Thrombosis and Haemostasis上发表了一篇研究文章,鉴于更多具有抗血栓作用的新型药物可能对COVID-19患者的治疗具有潜在效用,研究人员评估了正在进行包括这些药物在内及其在该人群中潜在作用机制的RCT。
 研究人员检索了clinical trials.gov和世界卫生组织国际临床试验注册平台,以确定COVID-19患者使用新型抗血栓药物的随机对照试验。
研究人员检索了clinical trials.gov和世界卫生组织国际临床试验注册平台,以确定COVID-19患者使用新型抗血栓药物的随机对照试验。
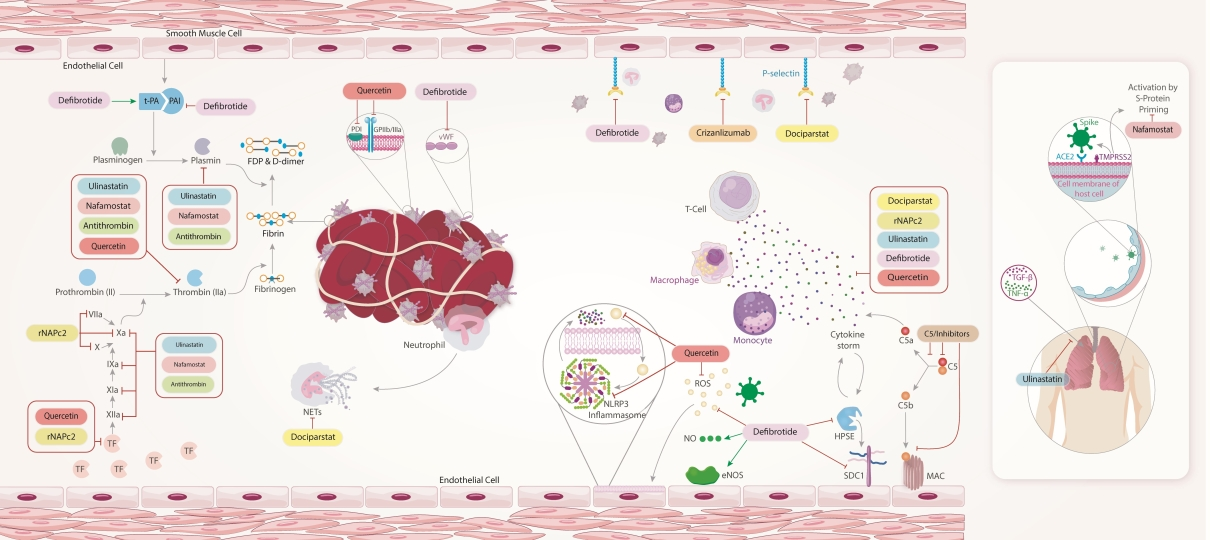
基于系统的文献检索,研究人员确定了27项RCT,其中包含10种新型抗血栓药物(包括萘法莫司他、多西帕司他、rNAPc2和去纤维肽)。这些试验的结果都尚未公布。这些正在进行的或已完成的RCT纳入的药物包括影响凝血级联反应、影响内皮激活和混合作用的药物。研究人员总结了他们假定的抗血栓形成机制及其对患者治疗的潜在效应。
由此可见,这些新型抗血栓药物具有多效抗炎和抗病毒作用,可能有助于降低病毒载量或纤维化,并改善患者氧合。正在进行的RCT的结果将阐明它们在COVID-19患者治疗中的实际效用。
原始出处:
Azita H. Talasaz.et al.Use of Novel Antithrombotic Agents for COVID-19: Systemic Summary of Ongoing Randomized Controlled Trials.Journal of Thrombosis and Haemostasis.2021.https://doi.org/10.1111/jth.15533
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#HAE#
37
#疗效分析#
34
#抗血栓药#
36
#抗血栓药物#
59
#抗血栓#
46
一直用的利伐沙班么
60
点赞,学习了
62
好文章,学习了。
58