Cell Death Dis:小檗碱对慢性溃疡性结肠炎的治疗作用
2020-05-10 QQY MedSci原创
溃疡性结肠炎(UC)是一种难治的慢性炎症性肠病(IBD),其特征是严重的腹泻、体重异常减轻、大便带血、腹痛和疲劳。 UC的炎症反应主要存在于结肠和直肠的粘膜和粘膜下层,其发病机制多样,且与遗传易感性、
尽管小檗碱(berberine,一种异喹啉生物碱)已被证实对实验性结肠炎具有保护作用,但其在慢性肠炎中的潜在分子机制仍不清楚。
该研究旨揭示了小檗碱在慢性UC中的治疗功效和免疫调节作用。
研究人员在DSS(葡聚糖硫酸钠)诱导的慢性UC小鼠模型中研究了服用小檗碱的治疗作用,并通过si-OSMR转染人肠道基质细胞的方式进一步验证其潜在的机制。
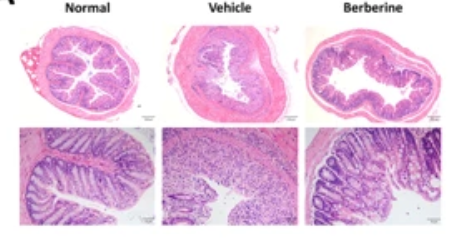
研究发现小檗碱可以显著减轻慢性UC的临床症状和肠道炎症反应。通过小檗碱治疗还可以维持肠屏障功能并改善组织纤维化。结合在结肠固有层中抗原呈递细胞(APC)、先天淋巴样细胞(ILC)和活化的NK细胞的浸润反应,在慢性UC炎症组织中发现OSM和OSMR的表达水平升高,小檗碱的治疗效果降低。此外,小檗碱可以通过调节OSM介导的JAK-STAT途径来抑制人肠道基质细胞的过度活化,而使用靶向OSMR的siRNA后该作用显著受到抑制。

该研究揭示了小檗碱的治疗机制,并发现通过干预OSM和OSMR的方式可能成为慢性UC的潜在治疗策略。
原始出处:
Li et al. Intervention of oncostatin M-driven mucosal inflammation by berberine exerts therapeutic property in chronic ulcerative colitis. Cell Death and Disease (2020) 11:271
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
42
#Cell#
48
#Dis#
40
#溃疡性#
35
#Death#
41