ARCH PATHOL LAB MED:钙化嵌套基质上皮肿瘤
2019-02-06 MedSci MedSci原创
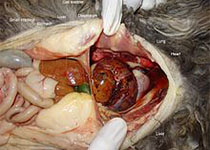
钙化嵌套间质-上皮肿瘤是一种少见疾病。该疾病在文献中有多种名称,如硬化性恶性混合上皮-间质肿瘤,硬化性间质-上皮肿瘤,以及肝纤维化嵌套梭形细胞瘤。据目前所知,文献报道的病例约有38例。组织发生尚不清楚,但组织病理学特征是梭形细胞和上皮样细胞巢呈器官样排列,周围有明显致密的肌成纤维细胞间质,偶见砂粒性钙化和局灶性异位骨化
钙化嵌套间质-上皮肿瘤是一种少见疾病。该疾病在文献中有多种名称,如硬化性恶性混合上皮-间质肿瘤,硬化性间质-上皮肿瘤,以及肝纤维化嵌套梭形细胞瘤。据目前所知,文献报道的病例约有38例。组织发生尚不清楚,但组织病理学特征是梭形细胞和上皮样细胞巢呈器官样排列,周围有明显致密的肌成纤维细胞间质,偶见砂粒性钙化和局灶性异位骨化。血管侵犯、肿瘤复发较为罕见,只有一个案例转移报告导致死亡。治疗主要是通过手术干预,化疗的作用似乎有限,但缺乏数据,因此正真的策略尚不清楚。排除肝母细胞瘤、钙化血管瘤、滑膜肉瘤、转移性胃肠道间质瘤、增生性小圆细胞瘤等影像学和病理组织学表现相似的病变非常重要。
原始出处:
Mark Benedict and Xuchen Zhang, Calcifying
Nested Stromal-Epithelial Tumor of the Liver: An Update and Literature Review
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Pathol#
24
#基质#
19
#上皮肿瘤#
25
#Med#
22
好
54
谢谢分享学习
51
学习了,谢谢分享
65