Radiology:三维MR弹性成像,做到慢性肝炎患者的“一站式”检查!
2021-08-23 shaosai MedSci原创
现阶段,慢性乙型肝炎(CHB)和丙型肝炎(CHC)仍然是全世界范围内的一个重要健康问题。在对这类患者进行诊治时,肝脏纤维化(LF)的严重程度是一项十分重要的评估手段。

现阶段,慢性乙型肝炎(CHB)和丙型肝炎(CHC)仍然是全世界范围内的一个重要健康问题。在对这类患者进行诊治时,肝脏纤维化(LF)的严重程度是一项十分重要的评估手段。多项研究证实,MR弹性成像是现阶段评估LF的最为准确的成像方法之一。
尽管弹性成像技术在对LF进行分期时具有优越性,但有研究发现,基于二维MR弹性成像的肝脏硬度(即剪切硬度[SS])也受炎症(如非酒精性脂肪性肝炎)或门静脉高压(PH)的影响。相比之下,多参数三维(3D)MR弹性成像允许组织的基本粘弹性建模,将复杂的剪切模量划分为弹性成分(如存储模量)和粘性成分(如损失模量和阻尼比[DR])。然而据我们所知,尚未有研究探讨三维MR弹性成像在CHB或CHC中的使用。
近日,发表在Radiology杂志的一项研究评估了多参数三维MR弹性成像在检测早期坏死性炎症、区分坏死性炎症和纤维化以及衡量CHB和CHC门静脉高压的严重程度方面的价值,为临床慢性肝炎患者准确诊治提供了影像学保障。
从2015年1月到2019年9月,本研究从一个机构中前瞻性地招募了CHB或CHC患者,并将其分为两组:有肝脏活检且无PH证据的患者(第1组)和有PH且肝静脉压力梯度(HVPG)测量的患者(第2组)。从附近的社区招募了健康志愿者作为第3组。使用60赫兹的三维MR弹性成像技术对多个粘弹性参数(剪切刚度[SS]、储能模量、损耗模量和阻尼比[DR])进行测定,并使用多变量逻辑或线性回归分析来评估机械参数与组织学评分和HVPG的关联。
第1组共有155名参与者(中位年龄,41岁[四分位数范围,32-48岁];85名女性),第2组有85名参与者(中位年龄,57岁[四分位数范围,43-61岁];51名女性),第3组有60名健康志愿者(中位年龄,49岁[四分位数范围,27-64岁];38名男性)。有坏死性炎症的参与者(DR,0.13 ± 0.03)与没有坏死性炎症的参与者(肝纤维化F0期)(DR,0.10 ± 0.02;P < .001)相比,肝脏DR更高。在验证数据集中,肝脏DR和SS在诊断坏死性炎症(受试者工作特征曲线下的面积[AUC],0.88[95% CI: 0.79, 0.96])和中度至重度活动评分(AUC,0.88[95% CI: 0.81, 0.95])方面表现良好。肝脏DR(回归系数[β] = -30.3 [95% CI: -58.0, -2.5]; P = .03)和脾脏SS(β = 2.3 [95% CI: 1.7, 2.9]; P < .001)与HVPG独立相关。
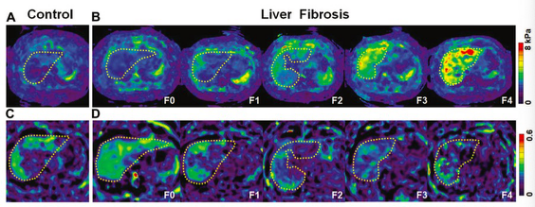
图 健康对照组和慢性乙型或丙型肝炎患者(用虚线勾勒的肝脏)的三维MR弹性成像图像。(A)对照组的肝脏剪切硬刚度(SS)图。(B) F0至F4期肝纤维化(LF)患者的肝脏SS图。(C) 对照组的阻尼比(DR)图。(D) F0到F4阶段的LF患者的DR图。
本研究表明,先进的三维(3D)MR弹性成像是一种简单、快速、有效的用于慢性乙型或丙型肝炎患者诊治评估的影像学手段,为临床提供了全面检测早期坏死性炎症、区分坏死性炎症和纤维化、并一次性测量门静脉高压的严重程度的有效工具,使得该类患者的个性化评估和医疗护理成为可能。
原文出处:
Yu Shi,Ya-Fei Qi,Gong-Yu Lan,et al.Three-dimensional MR Elastography Depicts Liver Inflammation, Fibrosis, and Portal Hypertension in Chronic Hepatitis B or C.DOI:10.1148/radiol.2021202804
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#MR弹性成像#
51
#一站式#
38
#弹性成像#
42
#肝炎患者#
54
#慢性肝炎#
44