ICM:ICU中血糖目标应该以平日血糖水平作为控制目标?
2022-01-01 ANDs 网络
NICE-SUGAR研究纳入了最多的患者,发现了几乎相反的结果,显示将血糖维持在180 mg/dL以下是有益的,而不是81-108 mg/dL范围内。此后,血糖维持在180 mg/dL以下一直被认为是
急性高血糖症可能是对应激的一种适应性反应。它通常发生在危重成人患者中,并与较差的临床结局相关。尽管在过去二十年中,许多临床试验都对血糖控制进行了研究,但危重成人的最佳血糖目标仍存在争议。Van den Berghe等人进行的前两个单中心试验发现,将血糖维持在正常范围内(即80至110 mg/dL)是有益的,而不是宽松的管理策略(即仅在血糖超过215 mg/dL时输注胰岛素,并将血糖维持在180至200 mg/dL之间)。然而,这些结果并未在多中心研究中得到证实。
NICE-SUGAR研究纳入了最多的患者,发现了几乎相反的结果,显示将血糖维持在180 mg/dL以下是有益的,而不是81-108 mg/dL范围内。此后,血糖维持在180 mg/dL以下一直被认为是重症监护病房(ICU)成人的常规血糖目标。然而,一些观察性研究表明,ICU中的血糖与低血糖或死亡率之间存在各种关系,这种关系取决于患者入院前的血糖,与非糖尿病患者相比,糖尿病患者在ICU期间的平均血糖与最低死亡率的相关性更高。这些观察结果与Van den Berghe等人进行的随机对照试验结果一致。该试验未发现把糖尿病患者的高血糖正常化的益处。因此,评估在ICU环境下使用个体化血糖目标的益处似乎很重要。
2021年11月来自法国的Julien Bohé等在Intensive Care Med上公布了CONTROLING研究结果,目的在于探讨针个体化的高血糖管理(根据入院前的血糖水平)是否能够改善患者的预后。
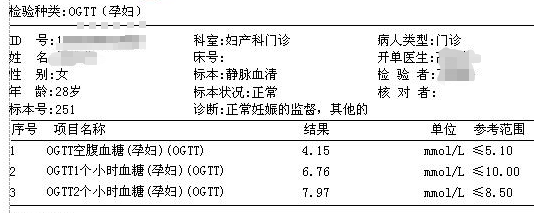
CONTROLING为多中心、随机、双盲、平行分组研究,纳入了成人危重症患者。直到患者ICU出院前,通过入院时糖化血红蛋白A1c水平来个体化地控制ICU血糖(IC组),或通过将糖血症维持在180毫克/分升以下控制血糖(CC组)。IC 组根据 A1C 水平计算平时血糖水平:平日血糖水平=28.7 × A1C-46.7 (in mg/dL, with A1C in %),IC 组血糖目标为平日血糖水平 + 15 mg/dL or less。主要结局为90天内死亡。
由于获益的可能性较低,且有证据表明低血糖的可能性,该研究被提前终止。随机了2075例;1917接受干预,其中 IC 组942例,CC组975例。
尽管两组在血糖控制方面存在显著差异,但90天的存活率并无显著差异(IC组:67.2%,95%可信区间[64.2%;70.3%];CC组:69.6%,95%可信区间[66.7%;72.5%])。IC组有3.9%的患者发生严重低糖血症(低于40毫克/分升),CC组有2.5%的患者发生严重低糖血症(p=0.09)。事后分析显示,与CC组相比,IC组非糖尿病患者90天死亡率的风险更高(HR 1.3,95%可信区间1.05;1.59,p=0.018)。
最终作者认为,与将糖血症维持在180毫克/分升以下相比,以ICU患者入院前的平日血糖水平为目标,使用动态滑模量表(dynamic sliding scale)的胰岛素方案并未发现生存的获益。
文献出处:
Intensive Care Med. 2021 Nov;47(11):1271-1283.
doi: 10.1007/s00134-021-06526-8. Epub 2021 Sep 29.
Individualised versus conventional glucose control in critically-ill patients: the CONTROLING study-a randomized clinical trial
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血糖水平#
38
学习
64
#控制目标#
39
很好,学习了
58
好好学习,天天向上
61