Oncologist:一例dMMR及种系BRAC1突变子宫内膜癌患者使用帕博利珠单抗达到完全缓解的病例报告
2018-03-07 慧语 肿瘤资讯
子宫内膜癌是常见的妇科恶性肿瘤,尽管大多数病例早期阶段可以根治。但晚期或转移的患者预后较差。一部分子宫内膜癌患者会呈现错配修复缺陷(dMMR)。dMMR的肿瘤患者对PD-1/PD-L1抑制剂治疗敏感,然而,BRCA1或BRCA2突变的患者,对PD-1抑制剂的敏感性知之甚少。此篇报告一例患有侵袭性体细胞dMMR并同时伴有BRAC1突变的子宫内膜癌患者,经帕博利珠单抗治疗后快速达到完全缓解。
子宫内膜癌是常见的妇科恶性肿瘤,尽管大多数病例早期阶段可以根治。但晚期或转移的患者预后较差。一部分子宫内膜癌患者会呈现错配修复缺陷(dMMR)。dMMR的肿瘤患者对PD-1/PD-L1抑制剂治疗敏感,然而,BRCA1或BRCA2突变的患者,对PD-1抑制剂的敏感性知之甚少。此篇报告一例患有侵袭性体细胞dMMR并同时伴有BRAC1突变的子宫内膜癌患者,经帕博利珠单抗治疗后快速达到完全缓解。
背景:
MSI-H/dMMR亚型在结直肠癌,子宫内膜癌,胃癌等类型中患者人数相对较多。这种亚型肿瘤的癌细胞中会出现大量DNA突变。因此,肿瘤如果进展到晚期,通常对化疗不敏感,而且由于DNA突变多,容易进化而产生耐药,因此传统上讲患者的预后较差。但随着PD1/PDL1抑制剂的出现,此类患者的治疗突然出现了曙光。
患者
女,42岁,2010年患IVB期霍奇金淋巴瘤,接受贝伐单抗加标准化疗(多柔比星,博来霉素,长春新碱和地塞米松)治疗,一年后复发。随后,对胸腔纵隔进行自体干细胞移植和巩固性放射治疗,2013年1月达到临床缓解。2015年1月,宫腔镜及刮宫术检查,出现不规则阴道出血,初步诊断为1级子宫内膜癌,给予全腹腔镜子宫切除术和双侧输卵管切除术,最终病理证实为T1B、1级子宫内膜样腺癌,伴有淋巴管浸润和阳性盆腔积液。
家族史:同父异母妹妹有霍奇金病和导管原位癌病史(BRCA突变测试为阴性);姑姑有乳腺癌病史;父母的叔叔均有前列腺癌病史。
在全面手术确认分期之前,发现一阴道结节,质坚实而柔软。2015年3月,接受盆腔和主动脉旁淋巴结清扫加阴道肿块切除术,病理显示所有淋巴结均为阴性;阴道切除术病理显示为子宫内膜样腺癌1级,认为是来自子宫内膜的移性病灶,MSH2和MSH6表达缺失,即dMMR。术后一个月影像随访,PET/CT显示右直肌和脐部出现转移性病灶(图1A)。鉴于之前接受过淋巴瘤治疗,2015年5月,使用醋酸甲地孕酮治疗3周+他莫昔芬疗程3周。3个月后,右直肌进展,阴道第二次发生复发,用放射疗法治疗腹壁病变,阴道,低骨盆及腹股沟盆腔,2015年11月完成放疗。期间试图将顺铂作为放射增敏剂,但因会延长骨髓抑制而最终放弃。2016年1月,接受腹壁病变切除术和根治性外阴切除术及外阴重建术,2016年5月,PET/CT显示会阴病变(图1B1-2),出现再次复发。重复活检显示肿瘤已经发展为高级别的苗勒氏腺癌。此次复发的组织学更具侵袭性,再次免疫组化检查仍显示为MSH2和MSH6表达缺失。进一步行基因组检测分析。

子宫内膜癌是最常见的妇科恶性肿瘤,在美国新发病例中超过6万例,其中大多数病例处于早期阶段,并且可以根治,但晚期、转移或复发的患者预后较差。尽管目前在一线(或辅助治疗)中已确定了有效的标准治疗方案,但二线或后续治疗方案选择还较为有限。因此,研究人员希望通过分子检测探索预测性生物标志物,为复发、晚期或转移性子宫内膜癌的患者提供新的策略。
基因分型和解读
对91个基因进行肿瘤基因组测序分析检测了多种突变,发现了包括BRCA2、TP53、PTEN和激活PIK3CA中的多种突变。12个变异体中,11个在单核苷酸重复中涉及C>T(或G>A)转变或小插入/缺失,这与MSI-H/dMMR肿瘤相关的突变签名一致。对BRCA1和MSH2进行种系突变检测,并在BRCA1中检测到致病性缺失。这种突变体也称为BRCA1 185delAG,,能够引起遗传性乳腺癌和卵巢癌综合症。
分子变换的功能意义
分子改造的临床意义和应用
有关dMMR肿瘤患者对免疫检查点抑制剂治疗获益的研究已经有很多。因此,高突变负荷肿瘤(TMB)患者将从PD-1抑制剂的治疗中益处。事实上,虽然对所有肿瘤类型的PD-1抑制剂反应的预测因子尚无定论,但对多种预测因素已进行了评估。在Diaz等人的研究中,86例dMMR患者应用帕博利珠单抗后客观缓解率为53%(完全缓解率为21%)。FDA最终依据该研究批准帕博利珠单抗用于MSI的所有肿瘤。BRCA1和BRCA2突变与同源重组缺陷相关,采用(铂类药物)化疗和其他DNA损伤以及PARP抑制剂等药物治疗后,癌细胞易于凋亡。然而,对于涉及同源重组的双链断裂DNA修复途径已知突变的患者对PD-1抑制剂的敏感性的了解还不够充分。与dMMR型肿瘤类似,BRCA突变也导致更高的TMB,这也可能使得肿瘤细胞易受由免疫检查点抑制剂引起的免疫介导的细胞毒性的影响。测序数据表明患者的子宫内膜肿瘤在BRCA1(种系)和BRCA2(体细胞)中具有致病性的突变。因此推测这两种基因的部分缺失可能导致BRCA修复途径的活性降低并进一步促成肿瘤新抗原的产生(图2)。
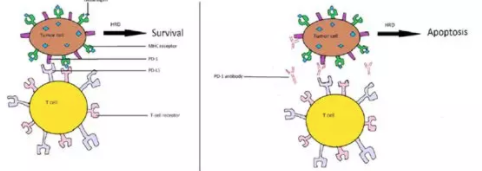
图2 提高对帕博利珠单抗敏感性的机制
更新
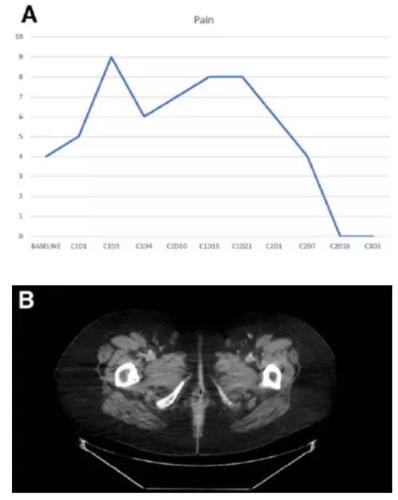
鉴于患者不能耐受顺铂作为放射增敏剂,不推荐选择全身治疗,同时患者对放射治疗抵抗,且不适合进行手术治疗。2016年6月,开始尝试帕博利珠单抗(2 mg/kg,每3周)。一次治疗后,肿瘤缩小30%,第三个疗程开始时,疼痛完全消失(图3A)。四个疗程后,影像显示会阴部肿瘤完全消失,达到完整缓解,且在治疗13个月后仍持续缓解(图3B)。
结论
此侵袭性BRCA1突变子宫内膜癌病例。致病性BRCA2突变发生在其dMMR的肿瘤上,会导致BRCA修复途径的部分损伤。但正是这种罕见情况的发生缺导致了该患者经PD-1抑制剂治疗后取得迅速和持续响应的结果,正可谓“山穷水复疑无路;柳暗花明又一村”。
关键点:
子宫内膜癌,特别是子宫内膜样癌,应行错配修复蛋白的免疫组化检测。
伴有dMMR的子宫癌患者建议采用PD-1抑制剂治疗。
对复发性、晚期或转移性肿瘤的基因检测可能有助于确定患者是否适合采取精准治疗。
原始出处:
Don S. Dizon, et al. Complete Remission Following Pembrolizumab in a Woman with Mismatch Repair‐Deficient Endometrial Cancer and a Germline BRCA1 Mutation. Oncologist. 2018 Feb 22. pii: theoncologist.2017-0526. doi: 10.1634/theoncologist.2017-0526.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






谢谢分享
52
#完全缓解#
29
#内膜#
31
#Oncol#
34
#帕博利珠#
34
学习了新知识
0
学习了新知识
48
学习了新知识
47
学习了新知识
48
学习了谢谢分享!!
33