Stroke:新技术——高级神经血管通路血栓切除系统治疗急性卒中安全有效!
2022-04-05 网络 网络
在这一临床经验中,ANA设备实现了较高的完全再通率,具有初步良好的安全性和有利的90天临床结果。
高级神经血管通路(ANA)血栓切除系统是一种新型的中风血栓切除装置,包括一个自我膨胀的漏斗,旨在通过局部限制血流来减少血栓的破碎,同时变得与所处的动脉一样宽。一旦展开,ANA设备允许远端抽吸,结合支架回收器,将血栓动员到漏斗中,在抽吸过程中,血栓仍被夹住。
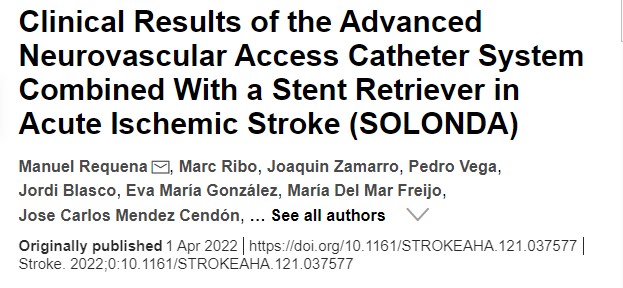
近期,来自西班牙巴塞罗那的学者开展了一项名为SOLONDA 前瞻性、开放式、单臂、多中心试验,旨在调查了ANA导管系统的安全性和有效性,结果发表在近期stroke杂志上。
该研究纳入所有卒中症状发生后8小时内入院的前循环血管闭塞患者符合条件。主要终点是在有意治疗的人群中,在使用抢救治疗之前,使用ANA设备结合支架取出器,成功进行再灌注(改良的脑梗塞溶栓评分2b-3)。主要的预定义分析是与HERMES(使用多种血管内设备的高效再灌注)中观察到的性能终点相比的非劣效性。
在招募了74名患者后,进行了中期分析,由于达到了安全和绩效目标,试验指导委员会决定终止招募。平均年龄为71.6(SD 8.9)岁,46.6%为女性,入院时美国国立卫生研究院卒中量表NIHSS评分中位数为14(IQR:10-19)。
60/72名患者在抢救治疗前的3个通道内成功实现了再灌注(83.3%[95%CI,74.7%-91.9%]),完全再灌注率(改良的脑梗塞溶栓评分2c-3)为60%(43/72; 95%CI,48.4%-71.1%)。在非劣效性得到确认后(P<0.01),ANA设备在≤3次的成功再灌注率方面也显示出优越性(P=0.02)。
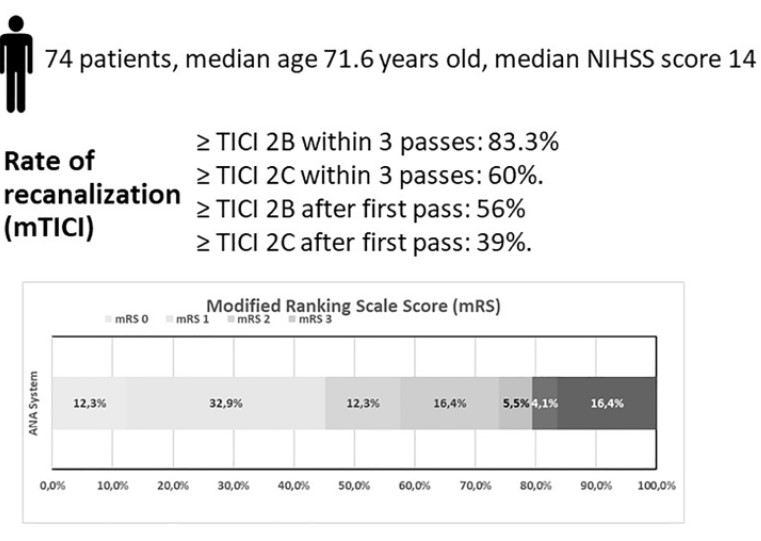
90天后画着mRS评分结局
总的来说,第一次成功再通率为55.6%(95%CI,44.1%-67.0%),第一次完全再通率为38.9%(95%CI,27.6%-50.1%)。12/72(17%)名患者需要进行抢救性治疗以获得修改后的脑梗塞溶栓评分2b-3。90天后,良好的功能结果(mRS 0-2)的比率为57.5%(95%CI,46.2%-68.9%),优秀的功能结果(mRS 0-1)比率为45.2%(95%CI,33.8%-56.6%)。
在这一临床经验中,ANA设备实现了较高的完全再通率,具有初步良好的安全性和有利的90天临床结果。
参考文献:
Clinical Results of the Advanced Neurovascular Access Catheter System Combined With a Stent Retriever in Acute Ischemic Stroke (SOLONDA). Stroke. 2022;0:10.1161/STROKEAHA.121.037577.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#新技术#
53
学习了
61
#急性卒中#
63
#血栓切除#
59
#血管通路#
50
#系统治疗#
47