Br J Anaesth:外科术后入ICU患者的虚弱程度与临床结局之间的关系:一项系统综述和Meta分析
2022-02-16 贵州医科大学 麻醉与心脏电生理课题组 “罂粟花”公众号
背景:
背景:术前虚弱可能是术后不良结果的有力预测指标。我们调查了外科术后入ICU患者的虚弱程度和临床结果之间的关系。
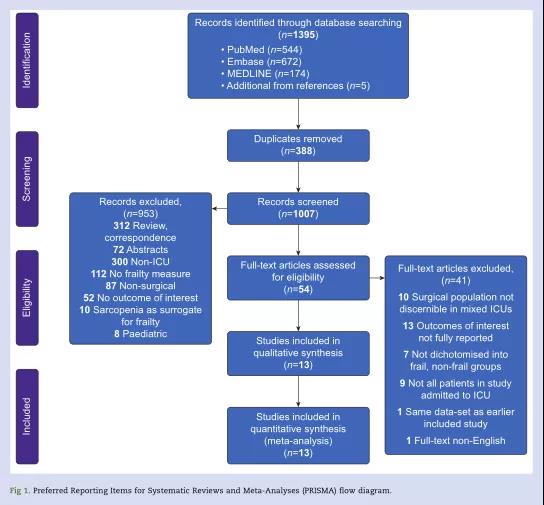
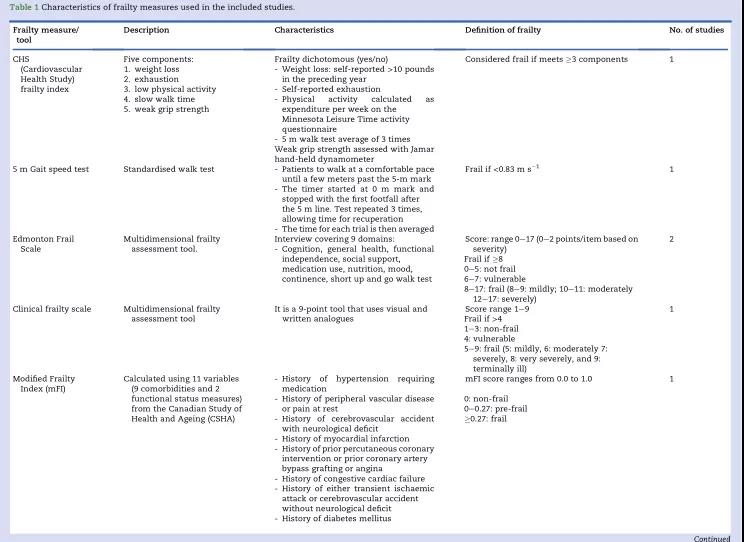
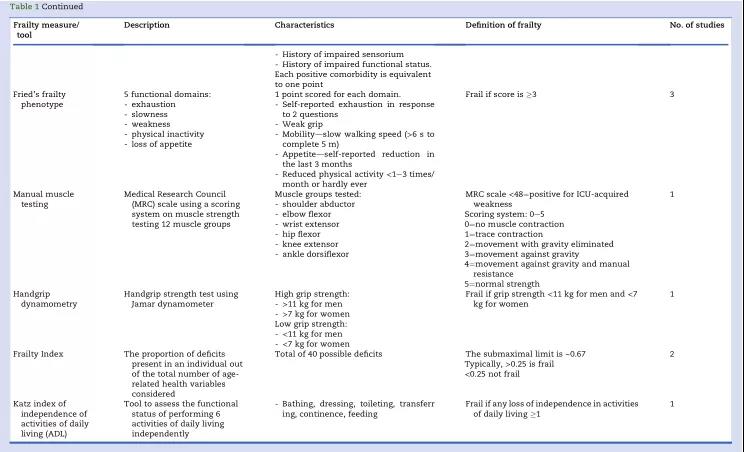
方法:我们检索了PubMed、Embase和Ovid MEDLINE数据库中收录的应用虚弱程度的相关文献原文。文献报导了术后入ICU成年(≥18岁)外科患者的结局,并以死亡率为主要观察指标。提取患者死亡率、机械通气时间、ICU和住院时间以及出院目的地的数据。纳入研究的质量和偏倚风险采用渥太华纽卡斯尔量表进行评估。根据系统综述和Meta分析指南的首选项目来综合处理数据。
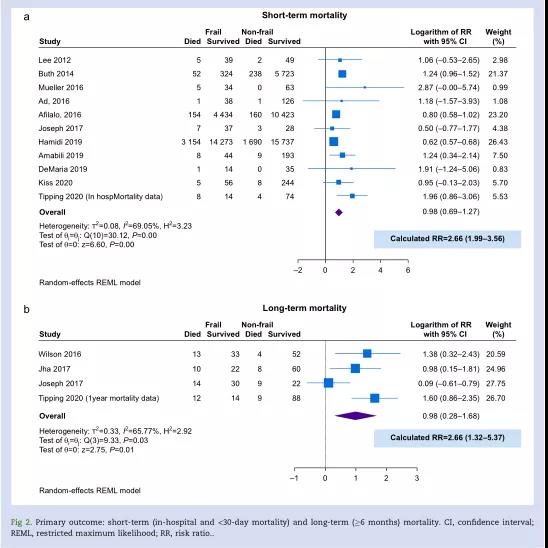
结果:共有13项观察性研究符合纳入标准。总共纳入58757名患者,其中22793名(39.4%)存在身体虚弱状况。虚弱与短期风险(风险比:2.66;95%可信区间[CI]:1.99-3.56)和长期死亡率(风险比:2.66;95%CI:1.32-5.37)相关。虚弱患者的ICU住院天数(均差[MD]=1.5天;95%CI:0.8-2.2)和住院天数(MD=3.9天;95%CI:1.4-6.5)较长。虚弱患者的机械通气时间更长(MD=22h;95%CI:1.7-42.3),而虚弱患者出院后也更大概率转运到医疗机构继续治疗(RR=2.34;95%CI:1.36-4.01)。
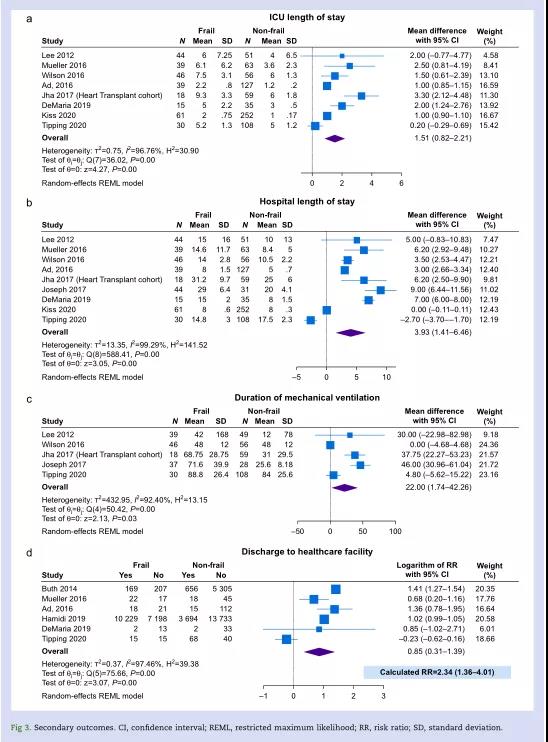
结论:因择期手术或急诊手术而需要术后入ICU的虚弱患者的死亡风险增加,住院时间延长,非家庭出院的可能性增加。术前虚弱评估和风险分层在患者与临床医生的计划,以及重症监护资源的利用中是必不可少的。
原始出处:
Rachel Chan, Ryo Ueno, Afsana Afroz, et al. Association between frailty and clinical outcomes in surgical patients admitted to intensive care units: a systematic review and meta-analysis. [J]Br J Anaesth, 128(2): 258-271(2022).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MET#
36
#ANA#
33
#Meta#
35
#系统综述#
43
#EST#
25
#临床结局#
36
学习了
39
#ICU患者#
36
有#虚弱量表#可以用
50