Nat Med:攻克靶向治疗耐药性,不给癌细胞复活的机会!
2018-11-29 vitam 转化医学网
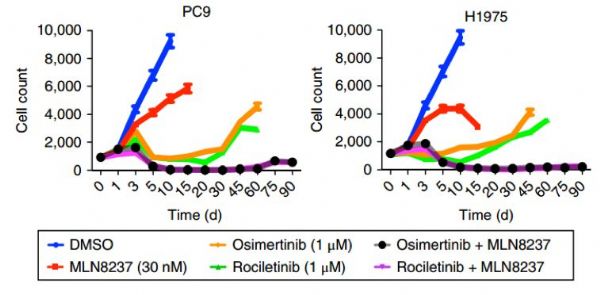
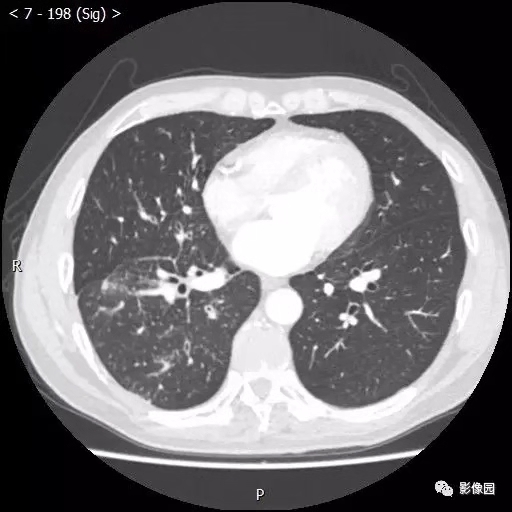
肺癌是发病率和死亡率增长最快、对人群健康和生命威胁最大的恶性肿瘤之一。近50年来许多国家都报道肺癌的发病率和死亡率均明显增高,男性肺癌发病率和死亡率均占所有恶性肿瘤的第一位,女性发病率占第二位,死亡率占第二位。而肺癌对靶向治疗产生耐药性是导致其死亡率居高不下的重要原因。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
29
学习学习谢谢
54
#癌细胞#
36
#Med#
32
越来越有希望了!
60
好
60
好好好好好好好好
51