Eur Heart J:晕厥对急性肺栓塞患者预后的不同影响
2018-10-22 xing.T MedSci原创
由此可见,晕厥作为急性PE的临床表现与出现血流动力学不稳定和RV功能障碍的患病率较高有关,并且早期PE相关不良结局的风险升高。与仅关注正常血压患者的研究相比,在包括未选择患者在内的研究中,晕厥与早期死亡风险增加的关联更为突出。
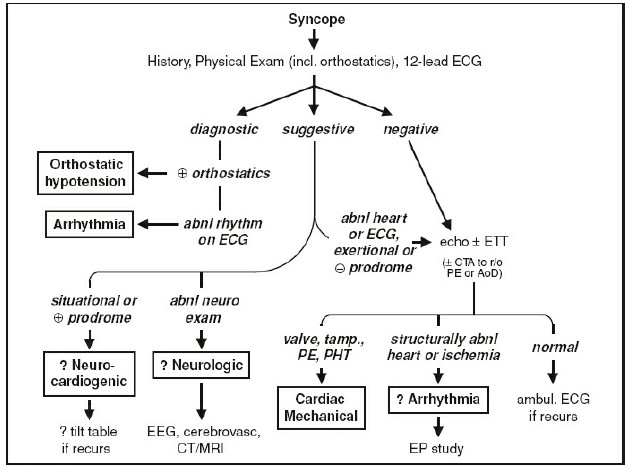
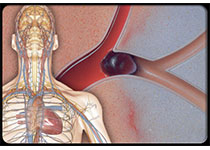
关于晕厥在急性肺栓塞(PE)患者中的预后作用和治疗意义的文献报道存在争议。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员进行了一项系统评价和荟萃分析,以调查晕厥与短期不良结局之间的关系,同时考虑了急性PE发生时血流动力学是否受损。
研究人员通过文献检索确定了1664项研究,其中纳入了29项研究共21956名PE患者(n=3706合并晕厥)。晕厥与血流动力学不稳定的患病率较高有关[比值比(OR)为3.50; 95%置信区间(CI)为2.67-4.58],以及发生时出现右心室(RV)功能障碍的超声心动图征象(OR为2.10; 95%CI为1.60-2.77)。晕厥患者早期(住院期间或30天内)死亡(OR为1.73;95%CI为1.22-2.47)和PE相关30天不良结局(OR为2.00; 95%CI为1.11-3.60)的风险较高。在包括未选择患者的研究中,全因死亡的绝对风险差异(95%CI)为6%(1%-10%),但在限制于血压正常患者的研究中为-1%(-2%至1%)。研究人员观察到晕厥在正式质量评估和回顾性评分较低的研究中没有预后效应。
由此可见,晕厥作为急性PE的临床表现与出现血流动力学不稳定和RV功能障碍的患病率较高有关,并且早期PE相关不良结局的风险升高。与仅关注正常血压患者的研究相比,在包括未选择患者在内的研究中,晕厥与早期死亡风险增加的关联更为突出。
原始出处:
Stefano Barco.et al. Differential impact of syncope on the prognosis of patients with acute pulmonary embolism: a systematic review and meta-analysis. Eur Heart J.2018. https://doi.org/10.1093/eurheartj/ehy631
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#患者预后#
38
#晕厥#
32
#急性肺栓塞#
39
#ART#
29
#HEART#
20