Cell Death Dis:lncRNA DOCK9-AS2促进甲状腺乳头状癌的发生发展
2020-09-17 QQY MedSci原创
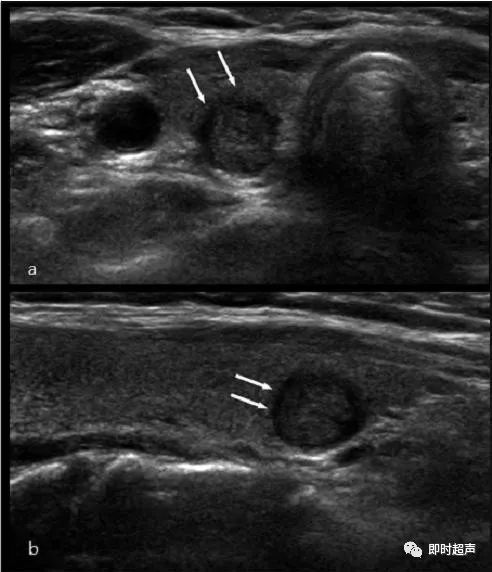
甲状腺乳头状癌(PTC)约占甲状腺癌(TC)总病例的80%。目前,PTC的治疗效果总体上令人满意,且超过95%的PTC患者在治疗后可以生存超过5年。但是,仍有约15%的PTC病例表现出侵袭性和不良预后
甲状腺乳头状癌(PTC)约占甲状腺癌(TC)总病例的80%。目前,PTC的治疗效果总体上令人满意,且超过95%的PTC患者在治疗后可以生存超过5年。但是,仍有约15%的PTC病例表现出侵袭性和不良预后。因此仍需改善PTC的诊断和靶向治疗策略。
目前的研究证实,长非编码RNA(lncRNA)能够介导肿瘤微环境中的细胞间通讯。 DOCK9-AS2是一种外泌体lncRNA,GEPIA和circlncRNAnet数据库中显示在甲状腺癌样本中DOCK9-AS2的表达水平上调,但尚无研究报道DOCK9-AS2在PTC中的功能和调节机制。
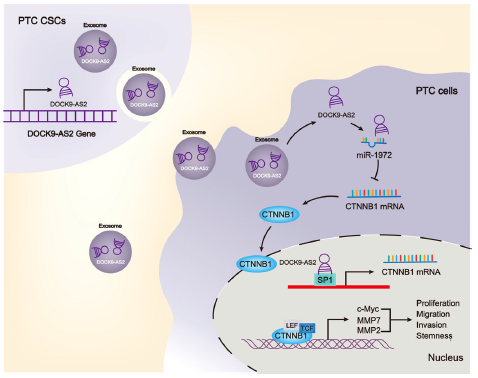
该研究通过生物信息学数据库分析PTC中差异表达的lncRNA,研究人员发现DOCK9-AS2在PTC中表达上调,且在PTC患者的血浆外泌体中含量升高。功能研究显示,敲低DOCK9-AS2可降低PTC细胞的增殖、迁移、侵袭、上皮-间质转化(EMT)和干细胞特性。研究人员进一步发现PTC肿瘤干细胞(PTC-CSC)能够通过外泌体呈递DOCK9-AS2来改善PTC细胞的干性。
机制研究显示,DOCK9-AS2能与SP1相互作用并诱导CTNNB1(连环蛋白β1)转录,且能够充当miR-1972的分子海绵上调CTNNB1的表达水平,从而激活PTC细胞中的Wnt/β-catenin信号通路。
总而言之,该研究揭示了PTC-CSC外泌体中的lncRNA DOCK9-AS2能够激活Wnt/β-catenin信号通路,并促进甲状腺乳头状癌的发生发展,说明DOCK9-AS2是PTC的一个潜在治疗靶标。
原始出处:
Dai, W., Jin, X., Han, L. et al. Exosomal lncRNA DOCK9-AS2 derived from cancer stem cell-like cells activated Wnt/β-catenin pathway to aggravate stemness, proliferation, migration, and invasion in papillary thyroid carcinoma. Cell Death Dis 11, 743 (11 September 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Dis#
40
#发生发展#
45
#CRN#
45
#CEL#
37
#乳头状#
39
#Cell#
32
#lncRNA#
46
#甲状腺乳头状癌#
32
#Death#
34