幽门螺杆菌(Helicobacter pylori),简称Hp,幽门螺旋杆菌,习惯性称为幽门螺杆菌、H.pylori,是一种革兰氏阴性的微需氧细菌,居于胃粘膜下和胃粘膜上皮之间,能活跃的侵入黏膜上皮细胞。

自1983年以来,科学家首次从慢性活动性胃炎患者的胃粘膜活检组织中将幽门螺杆菌分离成功后,是目前唯一能够在胃的强酸环境下生存下来的细菌。
诸多研究显示,幽门螺杆菌感染引发的胃炎、溃疡、胃癌等并发症的具体表现形式,同时也会引发十二指肠溃疡、胃肠息肉、结直肠癌,导致便秘、腹泻和体重减轻。根据美国卫生及公共服务部发布了第15版最新致癌物报告中,幽门螺杆菌被列为明确致癌物。

图:幽门螺杆菌感染引发的疾病
针对幽门螺杆菌的筛查方法,主要包括侵入式检查和非侵入式检查。侵入式检查包括内镜检查,可查看上消化道的任何异常情况并取出组织样本。非侵入式检查包括尿素呼气试验、血清抗体检测和粪便抗原检测,是目前临床常用的检测方法,被国内外多部幽门螺杆菌感染处理共识推荐。
其中,尿素呼气试验(UBT)是检测幽门螺杆菌的最常用的非侵入性方法,包括13尿素呼气试验(13C-UBT)和碳14尿素呼气试验(14C-UBT),该方法检测准确性和特异度相对较高、操作方便、不受幽门螺杆菌在胃内斑片状分布影响等优点,但在使用过程中,仍需要严格遵循检测流程,以确保检测结果的准确性。
那么,13C-UBT和14C-UBT有哪些区别,在临床中如何选择?本文整理汇总,以分享给同道学习。
1、尿素呼气试验原理
通常来说,胃内很少有细菌繁殖,没有尿素酶活性,而幽门螺杆菌富含尿素酶,能够将内源性和外源性的尿素分解为NH3和CO2,之后进入到血循环并由肺排出体外。
因此,口服一定剂量的同位素标记的尿素后,通过测定其呼出气体中同位素13C或14C标记的CO2变化情况,即可判断有无幽门螺杆菌感染。
2、 13C-UBT和14C-UBT的区别
呼气试验目前有两种示踪剂,即13C-尿素和14C-尿素。13C为稳定同位素,无辐射作用,但价格较高。14C的半衰期较长,价格较低,但有一定的辐射作用。
13C-UBT采用质谱分析方法进行检测分析,其测定值为收集受检者服药前和服药后的两个呼气样本进行对比测量。而14C-UBT通过液闪检测法,只对受检者服药之后的呼气样本进行测量。
13C-尿素剂量越高,13C-UBT检测准确性越高,但相应的成本会增加。 75mg剂量的平均敏感度和特异度均达到7% 以上,其足够高的准确性使其更为国内外专家临床上所推荐。欧洲药品评估局指南建议,对于13C-UBT 中的13C⁃尿素剂量,成人剂量为75mg,儿童剂量为45mg。而14C-UBT 中的14C⁃尿素剂量,患者只需口服 1粒14C标记尿素胶囊之后对集气装置吹气,胶囊剂量为27.8kBq(0.75μCi)/粒。
3 、13C-UBT和14C-UBT适应症
13C-UBT临床应用的范围包括抗幽门螺杆菌治疗后的复查 ; 有消化性溃疡史 , 但幽门螺杆菌状态不明者以及45岁以下有消化不良者。
14C-UBT适用于:1)消化不良初诊者、复诊者; 2)胃十二指肠溃疡、慢性活动性胃炎、胃窦炎; 3)相关性淋巴组织的淋巴瘤等需要根除幽门螺杆菌的患者; 4)预防胃癌或有胃癌家族史者; 5)胃镜检查有胃部不适的患者; 6)不愿意接受胃镜检查而有胃部不适的患者; 7)长期服用非甾体抗炎类药物者。
因此,检测幽门螺杆菌,到底选13C-UBT还是14C-UBT,医生可根据患者情况酌情选择。除孕妇、哺乳期妇女和儿童外,这两种尿素呼气试验的区别不大。
4 、尿素呼气试验的注意事项
UBT是幽门螺杆菌检测及根治后疗效监测,在临床上应用十分广泛。然而其检测的效能依旧受到诸多临床因素的影响,比如药物使用、检测仪器及检测试剂、检查者操作、饮食、以及疾病等。
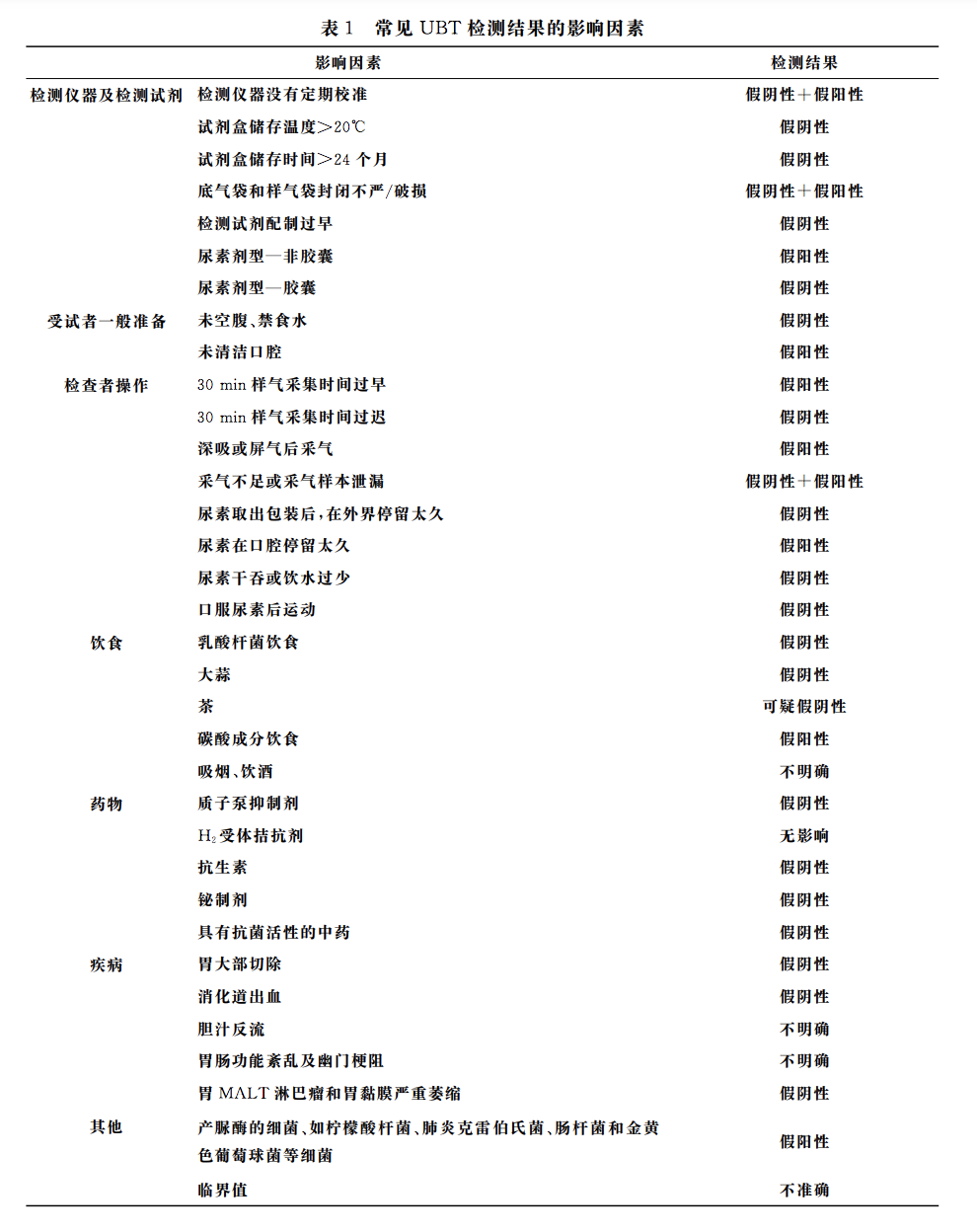
因此,在临床应用过程中应当避免这些影响,尽可能的使检查更精确,以提高诊断的准确率,更好的服务临床指导治疗。
参考资料
1.中华医学会消化病学分会, 中华医学会消化内镜学分会. 13C尿素呼气试验质量控制专家建议[J]. 中华消化内镜杂志, 2021, 38(3):4.
2.国家消化系疾病临床医学研究中心(上海), 国家消化道早癌防治中心联盟, 中华医学会消化病学分会幽门螺杆菌和消化性溃疡学组,等. 中国居民家庭幽门螺杆菌感染的防控和管理专家共识(2021年)[J]. 中华消化杂志, 2021, 41(4):13.
3.刘懿, 钟良, 孙大裕. 幽门螺杆菌感染的诊断——^13C—尿素呼气试验[J]. 国际消化病杂志, 2003, 23(002):85-87.
4.黄昊, 程中伟. 13 C呼气试验原理及临床应用[J]. 医疗卫生装备, 2003(S1):1.
5.白涛, 侯晓华. 尿素呼气试验检测幽门螺杆菌感染的影响因素[J]. 临床消化病杂志, 2020, 32(3):6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#螺杆菌#
68
学习了
51
感谢分享。
59
学习了,讲解的很好!
49
认真学习~~
58
签到
57