JCEM:轻度原发性甲状旁腺功能亢进和甲状旁腺切除术对动脉硬化的影响
2021-03-23 MedSci原创 MedSci原创
轻度pHPT患者主动脉僵硬度增加,该结果支持轻度pHPT与不良心血管表现存在相关性的观点。PTX可显著降低轻度pHPT患者的动脉僵硬度,这表明PTX对心血管症状的益处不应被忽视,值得进一步研究。
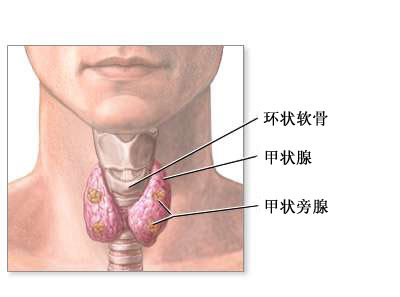
目前关于轻度原发性甲状旁腺功能亢进(pHPT)患者心血管系统临床表现的资料常常相互矛盾。脉搏波速(PWV)是评估主动脉僵硬度的金标准,可以预测心血管疾病的发病率和死亡率。

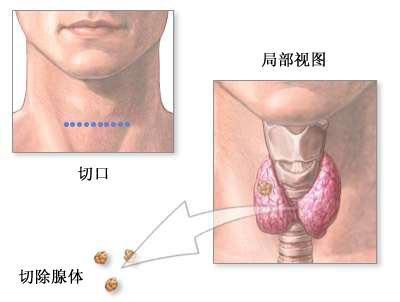
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究主要目的是调查轻度pHPT是否与高PWV相关,以及甲状旁腺切除术(PTX)是否降低了轻度pHPT患者的PWV。次要目的是调查PTX术后血压的变化情况。
研究人员检索了PubMed、谷歌Scholar、SCOPUS、Web of Science和Cochrane图书馆。符合条件的研究报道了轻度pHPT患者和对照者PWV情况,或在PTX前后的轻度pHPT患者PWV情况。两位研究者独立鉴定了符合条件的研究并提取了数据。合并平均差(MD)是总结性的效果指标。合并数据通过伴有异常值和有影响的案例诊断值的森林图进行呈现。

研究人员选择了9项观察性研究和1项RCT,包含433例轻度pHPT患者,其中171例接受PTX治疗,407例对照者。轻度pHPT患者的PWV显著高于对照者(MD=1.18, 0.67~1.68, p<0.0001)。7项研究评估了PTX对PWV的影响。PTX可显著降低PWV (MD=-0.48、-0.88至-0.07,p=0.022)。
由此可见,轻度pHPT患者主动脉僵硬度增加,该结果支持轻度pHPT与不良心血管表现存在相关性的观点。PTX可显著降低轻度pHPT患者的动脉僵硬度,这表明PTX对心血管症状的益处不应被忽视,值得进一步研究。
原始出处:
Stella Bernardi.et al.Meta-analysis on the effect of mild primary hyperparathyroidism and parathyroidectomy upon arterial stiffness.JCEM.2021.https://doi.org/10.1210/clinem/dgab157
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#切除术#
31
可以关注
41
#动脉硬化#
105
#JCE#
31
#JCEM#
34
#原发性#
26
#甲状旁腺功能亢进#
38
#甲状旁腺#
28
#甲状旁腺切除术#
38
#原发性甲状旁腺功能亢进#
23