Blood:联合抑制Bcl2和NFκB可协同诱导CTCL细胞死亡、限制其肿瘤生长
2019-06-06 QQ MedSci原创
皮肤T细胞淋巴瘤(CTCL)的治疗方法有限,目前尚无治愈方案。因此,亟需新的靶向性和耐受性良好的治疗方法。近期,Tabea C. Froehlich等研究人员发现二甲基甲酰胺(DMF)可抑制NFκB作为CTCL的存活因子。与此相似,抑制抗凋亡蛋白Bcl2也表现出可诱导CTCL细胞死亡,特别是当与HDAC抑制剂联合使用时。因此,研究人员推测在CTCL的一种新的联合治疗方案中,抑制Bcl2或可以增强对
近期,Tabea C. Froehlich等研究人员发现二甲基甲酰胺(DMF)可抑制NFκB作为CTCL的存活因子。与此相似,抑制抗凋亡蛋白Bcl2也表现出可诱导CTCL细胞死亡,特别是当与HDAC抑制剂联合使用时。因此,研究人员推测在CTCL的一种新的联合治疗方案中,抑制Bcl2或可以增强对NFκB的抑制作用,对此进行研究。
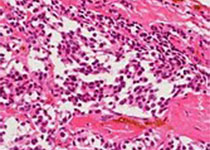
结果发现,在体外时,Bcl2抑制剂ABT-199和ABT-263可特异性诱导CTCL患者来源的原发性CD4+细胞死亡,在CTCL细胞系SeAx中具有相同结果,但对于健康供体的T细胞和缺乏Bcl2的CTCL细胞系HH则无此效应。ABT-199和DMF联合治疗可协同特异性诱导CTCL细胞死亡,ABT-199和DMF作用于两条独立的信号通路。
在体内,给予CTCL移植瘤小鼠模型ABT-199和DMF联合治疗可协同诱导CTCL细胞死亡和抑制肿瘤细胞增殖,进而有效减少肿瘤的生长、延长小鼠的总体存活期。无论是从疗效还是耐受性来看,这种联合治疗方案均优于ABT-199单药治疗。
综上所述,本研究表明Bcl2抑制剂和NFκB抑制剂联合具有极大的治疗CTCL的潜能,值得进一步开展研究来进行验证。
Tabea C. Froehlich, et al.Combined inhibition of Bcl-2 and NFκB synergistically induces cell death and limits xenograft mouse tumor growth in CTCL. Blood 2019 :blood.2019001545; doi: https://doi.org/10.1182/blood.2019001545
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TCL#
31
#NFκB#
20
#CTC#
39
#BCL2#
33