Movement Disorder: 神经丝轻链,可预测多系统萎缩症的病情进展
2022-01-14 Freeman MedSci原创
血浆NFL是衡量MSA疾病严重程度和监测MSA进展的可靠生物标志物
多系统萎缩(MSA)是一种罕见的成人发病的进行性神经退行性疾病,其特点是自身调节减弱、帕金森症、小脑共济失调和锥体征的不同组合。
 MSA进展迅速,没有有效的治疗方法;中位生存时间约为6至10年。据报道,基线时症状持续时间较短和对左旋多巴无反应预示着疾病的快速进展。
MSA进展迅速,没有有效的治疗方法;中位生存时间约为6至10年。据报道,基线时症状持续时间较短和对左旋多巴无反应预示着疾病的快速进展。
以自主神经功能紊乱为初始症状的患者和女性MSA患者的疾病进展更快。除了MSA中常见的自律神经功能障碍的非运动症状外,认知障碍也不罕见。
在MSA中除了运动功能恶化外,还观察到明显的认知能力下降。目前迫切需要能够预测MSA进展的生物标志物。
神经丝轻链(NFL)作为神经退行性疾病中轴索损伤的候选生物标志物,不仅在脑脊液(CSF)中,而且在血清中也越来越受到关注。
已有研究表明,MSA患者的血浆NFL高于帕金森病患者和健康对照组(HCs)。然而,缺乏关于NFL水平与MSA的严重程度和进展之间关系的研究。
藉此,华西医院的Lingyu Zhang等人,检查了MSA患者的血浆NFL水平,以研究血浆NFL水平是否与MSA严重程度相关,并阐明血浆NFL与MSA进展之间的关系。
MSA患者是一项前瞻性队列研究的一部分,在基线和1年后进行评估。使用超灵敏的Simoa技术对血浆NFL进行量化。
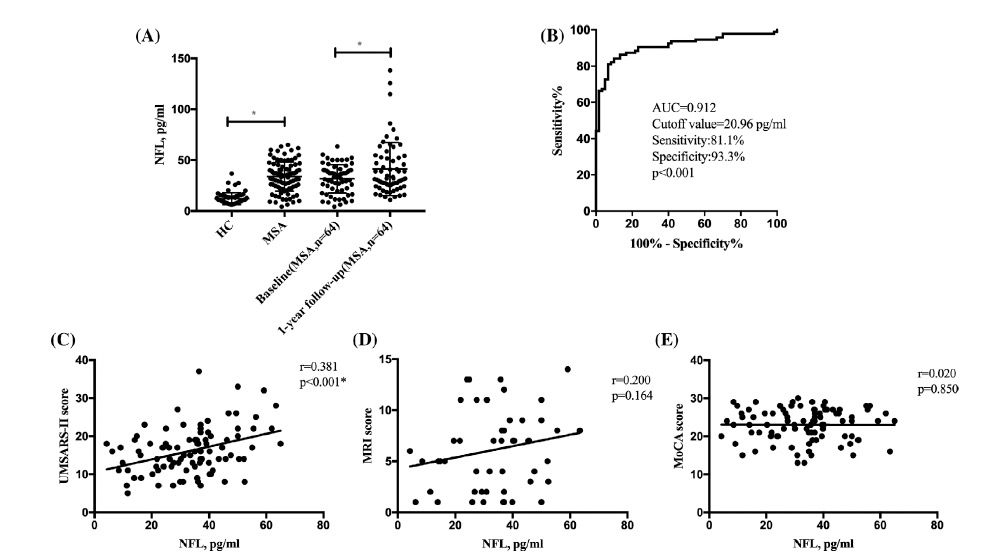
共有91名MSA患者和60名健康对照组(HCs)参加了研究。从基线到1年的随访中,NFL的水平有所增加(P = 0.010)。基线血浆NFL水平与MSA患者的运动严重程度和病情进展明显相关(P < 0.05),但与认知进展无关(P > 0.05)。
该研究的重要意义在于发现了;血浆NFL是衡量MSA疾病严重程度和监测MSA进展的可靠生物标志物,但与认知进展无关。
原文出处:
Zhang L, Cao B, Hou Y, et al. Neurofilament Light Chain Predicts Disease Severity and Progression in Multiple System Atrophy. Mov Disord. Published online October 31, 2021:mds.28847. doi:10.1002/mds.28847
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#disorder#
39
#Disord#
39
#Dis#
26
#病情#
30
#神经丝#
35
#神经丝轻链#
24
#萎缩#
25
#多系统萎缩#
48