中国研发出上消化道肿瘤内镜AI辅助诊断系统,敏感性超九成
2019-10-08 郑澍 央广网
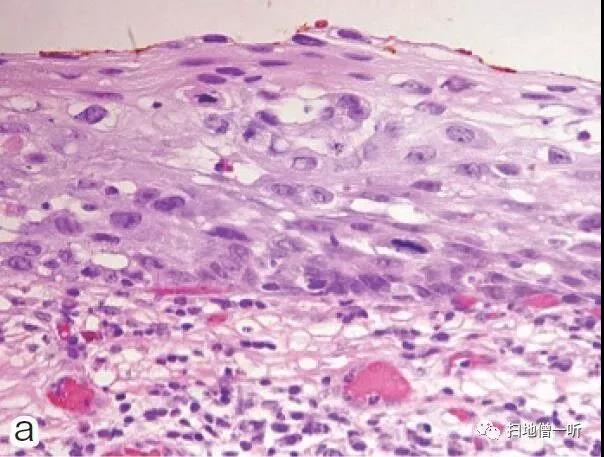
央广网广州10月8日消息 中山大学肿瘤防治中心专家团队成功自主研发出具有完全自主知识产权的上消化道癌内镜AI辅助诊断系统。经临床实践数据验证,对上消化道肿瘤的诊断敏感性高达90%以上。这一研究成果日前发表在肿瘤学顶尖期刊《柳叶刀·肿瘤》上。上消化道癌的早期诊断早期治疗是提高疗效的关键。目前,内镜检查及活检仍是上消化道癌早期诊断的金标准。但是我国的内镜医生十分短缺,人才缺口巨大,远远不能满足临床实际
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#上消化道#
37
#内镜#
25
#研发#
21
#敏感性#
31
#消化道#
25