Mol Cell:华人科学家首次发现二甲双胍可降解PD-L1,解除癌细胞对免疫细胞的压制,提高抗癌能力
2018-08-18 奇点糕 奇点网
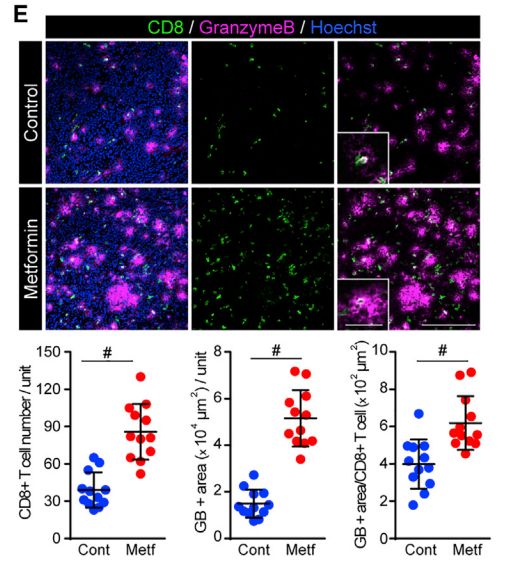
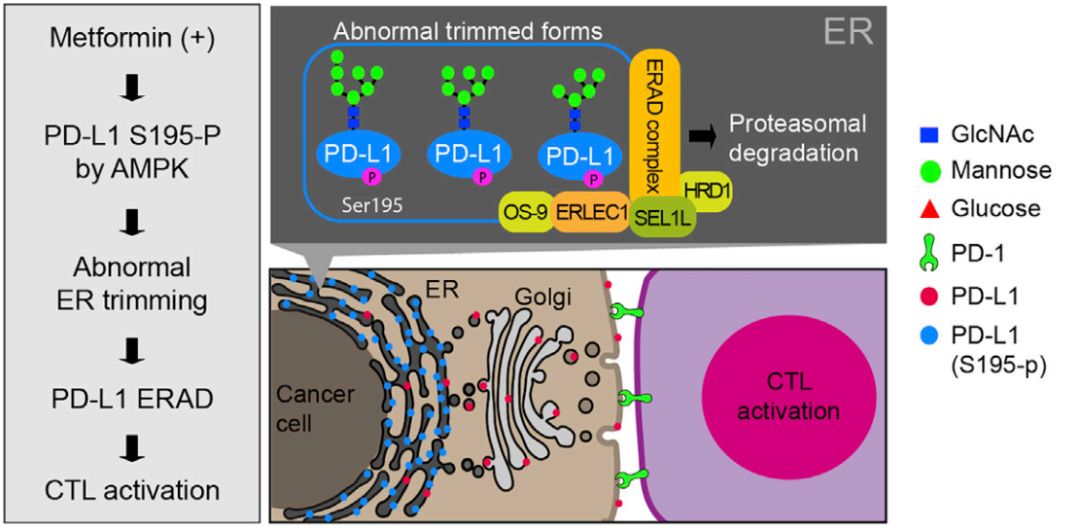
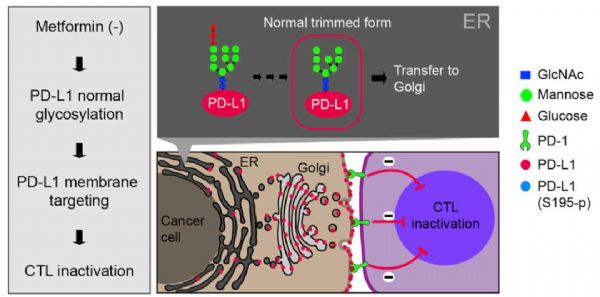
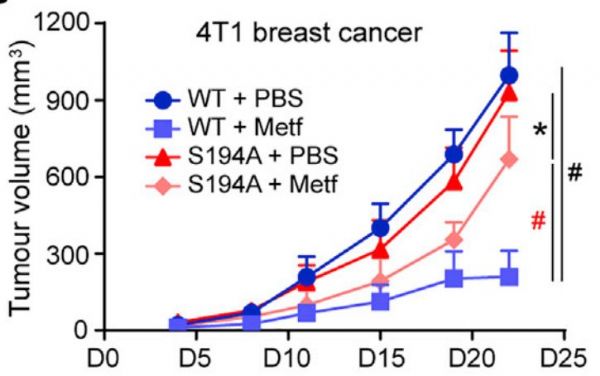
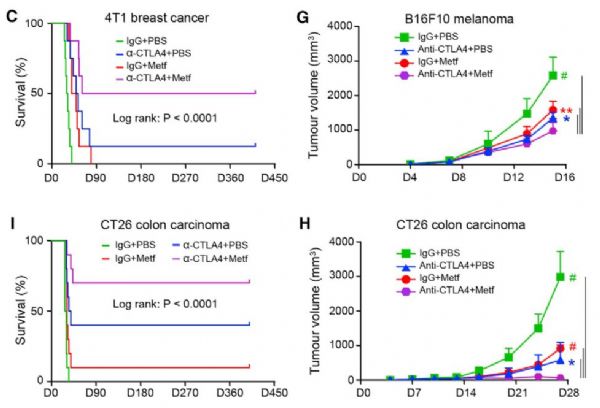
本周《分子细胞》杂志上刊登了MD Anderson癌症中心华人学者洪明奇(Mien-Chie Hung)团队的最新研究成果,二甲双胍竟然能够导致癌细胞表达的PD-L1降解,避免它们“逃脱”免疫系统的“搜查”!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Cell#
27
#CEL#
35
#癌细胞#
30
#PD-L1#
36
#华人#
34
学习了谢谢分享
61