Int J Cardiol:光学相干断层扫描和C-反应蛋白在急性冠状动脉综合征危险分层中的应用
2019-01-20 xing.T MedSci原创
由此可见,在罪犯斑块中炎症和OCT发现的系统证据的组合确定了非常高风险的ACS。未来的研究有必要证实这些发现并在该患者亚组中测试抗炎治疗。
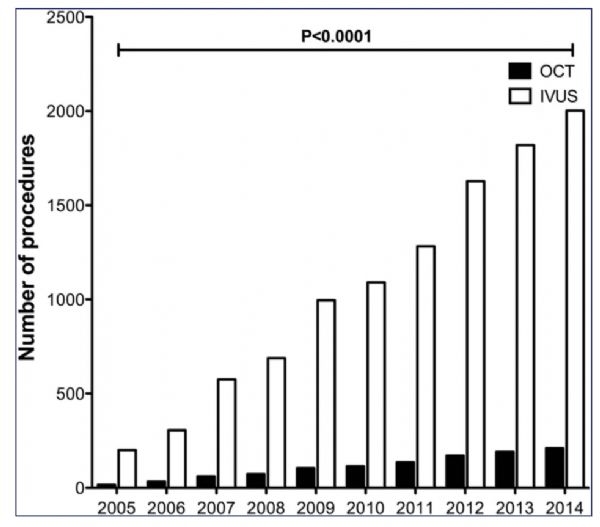
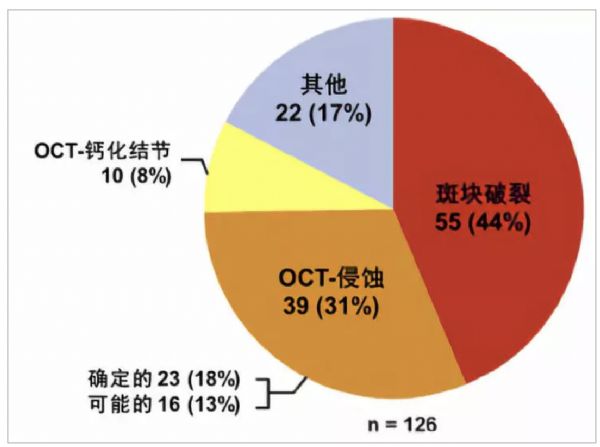
高C-反应蛋白(CRP)水平相关的急性冠状动脉综合征(ACS)患者表现出更高的急性缺血事件风险。然而,CRP的阳性预测值太低而无法指导特定治疗。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,研究人员旨在通过结合光学相干断层扫描(OCT)评估罪犯血管和CRP血清水平,确定可能主要受益于抗炎治疗的高风险患者亚组。
因ACS住院并接受罪犯血管的介入前OCT评估的患者均选自阿戈斯蒂诺医院OCT登记中心。该研究的主要终点是复发性ACS。CRP水平≥2mg/L被认为是异常的。
总体研究人群包含了178名患者。其中,156名患者被纳入主要终点分析。3年随访时再次发生ACS的比例为23%。高CRP(2.587,95%CI为1.345-10.325,p=0.031)、斑块破裂(3.985,95%CI为1.698-8.754,p=0.009)、巨噬细胞浸润(3.145,95%CI为1.458-9.587,p=0.012)和多灶性动脉粥样硬化(2.734,95%CI为1.748-11.875,p=0.042)是再次发生ACS的独立预测因子。所有具有较高CRP且具有所有OCT高风险特征的患者(14/14)都再次发生ACS。另一方面,82例CRP水平低且OCT缺乏高风险特征的患者中只有4例在随访时再次发生ACS。
由此可见,在罪犯斑块中炎症和OCT发现的系统证据的组合确定了非常高风险的ACS。未来的研究有必要证实这些发现并在该患者亚组中测试抗炎治疗。
原始出处:
FrancescoFracassi,et al.Optical coherence tomography and C-reactive protein in risk stratification of acute coronary syndromes.International Journal of Cardiology.2019.https://doi.org/10.1016/j.ijcard.2019.01.058
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#冠状动脉综合征#
40
#危险分层#
41
#Cardiol#
39
#综合征#
0
#C-反应蛋白#
38
#光学相干断层扫描#
37
学习了,谢谢分享
78