重症丘脑出血破入脑室1例
2018-10-22 詹燕 荀雅晶 王珊珊 神经损伤与功能重建
色素性神经鞘瘤(MS)起源于Schwann细胞,是一种起源于神经嵴且具有双向分化潜能的原始细胞肿瘤,以颈段和上胸段脊神经最为常见,因其可以产生黑色素故而在临床上容易误诊为恶性黑色素瘤。我科收治1例病理确诊的颈椎髓外硬膜下色素性神经鞘瘤病例,报告如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



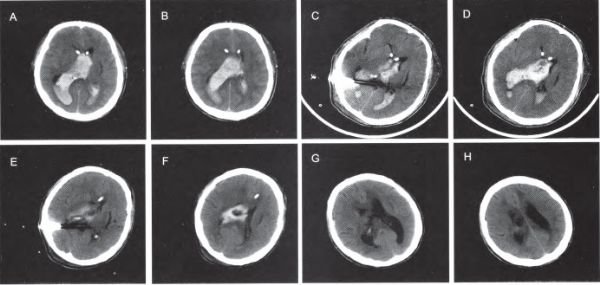








#丘脑出血#
38
#破入脑室#
33
#丘脑#
33
#丘脑#
39
#脑室#
35