Science:一个“非常规” 实验重写了我们对胃肿瘤的认识
2018-07-29 佚名 生物通
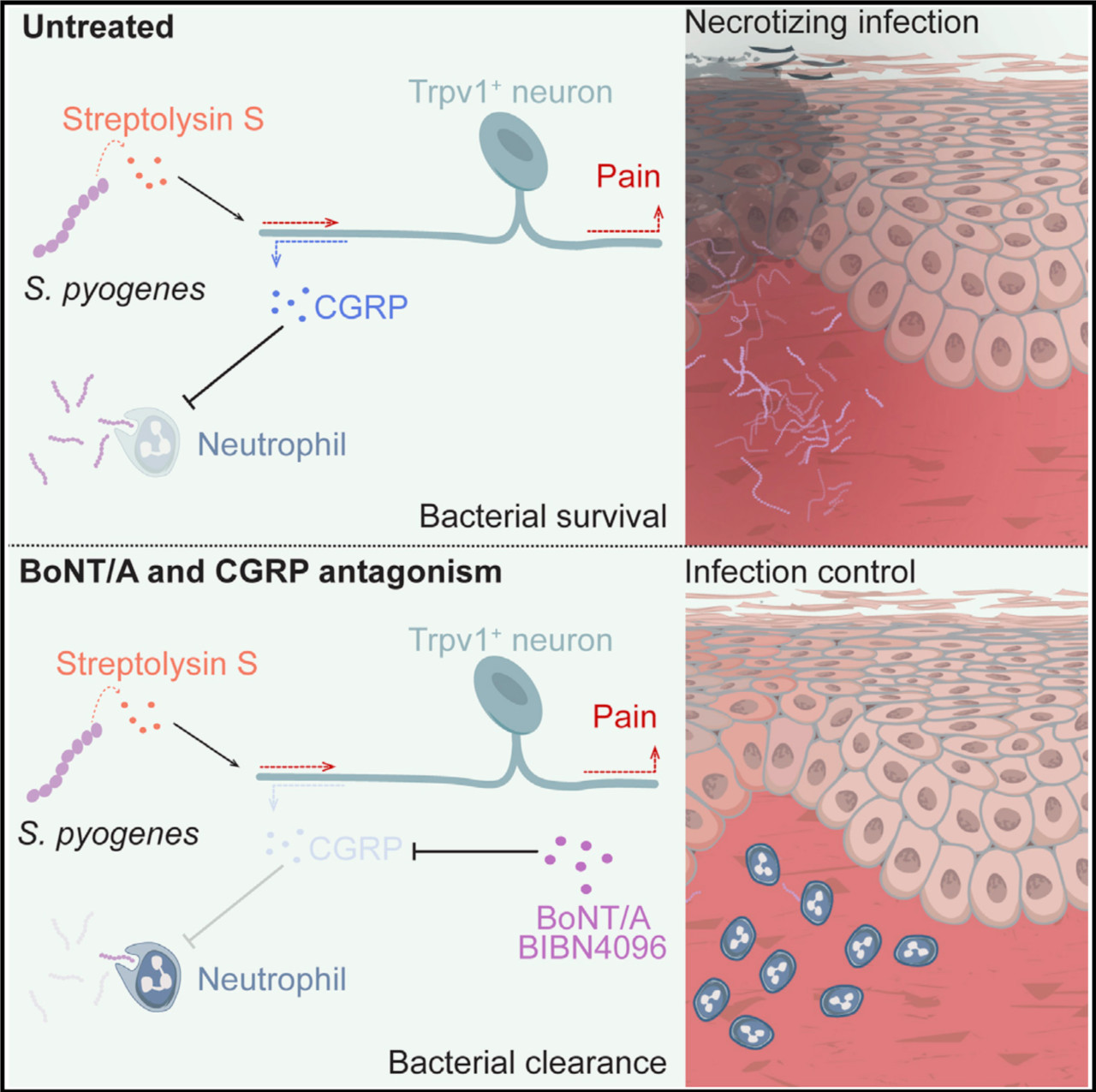
免疫系统是抗癌的重要盟友?近日《Science》杂志一项研究指出,免疫系统引发的异常炎症可能是一种遗传学癌症综合征“黑斑息肉综合征(Peutz-Jeghers Syndrome,PJS)”的致病基础。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#胃肿瘤#
35
炎症和PJS有关。
63
好资料学习了!
67
#SCIE#
29
学习了,长知识
63
了解一下谢谢
60