产前超声诊断肠旋转不良伴中肠扭转 1 例
2019-11-19 李琪 吴海芳 陶国伟 现代妇产科进展
孕妇, 29 岁, G1P0,孕 34 周于外院行超声检查提示:胎儿 上腹部脊柱前方偏右侧见“C 字型”肠管扩张,范围约3.6cm× 1.2cm,其背侧可见血管回声,有旋转感。孕妇唐筛未见异 常,未行无创及羊水穿刺检查,无家族病史。2018 年 7 月 31 日患者孕 37 周时于我院行产科超声检查,超声示: 单活胎, 胎儿测值符合孕周,羊水指数 15.1cm; 胎儿部分肠管迂曲扩 张,较宽处内径
1 病例简介
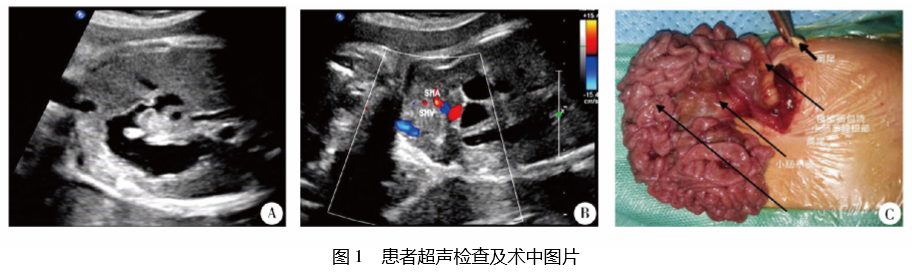
孕妇, 29 岁, G1P0,孕 34 周于外院行超声检查提示:胎儿 上腹部脊柱前方偏右侧见“C 字型”肠管扩张,范围约3.6cm× 1.2cm,其背侧可见血管回声,有旋转感。孕妇唐筛未见异 常,未行无创及羊水穿刺检查,无家族病史。2018 年 7 月 31 日患者孕 37 周时于我院行产科超声检查,超声示: 单活胎, 胎儿测值符合孕周,羊水指数 15.1cm; 胎儿部分肠管迂曲扩 张,较宽处内径 1.3cm( 图 1A) ,扩张肠管近端与胃泡相通, CDFI 显示远端肠系膜上静脉呈“螺旋状”缠绕于肠系膜上动 脉,略呈“漩涡征” ( 图 1B) 。超声示: 胎儿部分肠管扩张( 肠 旋转不良待排) 。2018 年 8 月 15 日孕妇孕 39 周,自然分娩 一男婴, 1、 5min Apgar 评分均为 10 分,体重 2.590kg,出生无 窒息,肠鸣音正常,脐带、胎盘、羊水未见异常。转至小儿内
科,给予喂养,反复呕吐,无腹胀。禁食,持续胃肠减压,引流 出大量黄色及黄绿色黏液。完善腹部立位片及消化道造影 检查,胃十二指肠处呈“双泡征”,小肠充盈。行钡剂灌肠检 查,可见盲肠、升结肠、横结肠肝曲向左中上腹堆积、聚拢,肠 管粗细尚均匀,横结肠偏右侧可见一阑尾显影,提示先天性 结肠分布发育不良。2018 年 8 月 23 日转入小儿外科行手术 治疗,术中见阑尾位于右中上腹,小肠系膜短、窄,逆时针扭 转 270°,肠管血运、颜色尚可,回盲部有纤维索带附着于右侧 腹壁,但压迫不明显,十二指肠、空肠连接部折角,十二指肠 第一、二、三段明显扩张( 图 1C) 。术后诊断: 肠旋转不良伴 中肠扭转。2018 年9 月7 日患儿因“呕吐一天”再次入院,腹 部立位平片显示未见明显气液平,予以补液、灌肠、胃肠减 压、理疗等对症治疗后好转出院,至今患儿情况好。
A:胃泡与近端扩张肠管; B:远端肠系膜上静脉呈“螺旋状”缠绕于肠系膜上动脉,略呈“漩涡征” ; C:术中所见,小肠系膜短窄,逆时针扭转 270°,肠管血运、颜色尚可
2 讨 论
先天性肠旋转不良是胚胎期肠发育过程中受致畸因素 的影响,以肠系膜上动脉为轴心的正常旋转运动发生障碍, 使肠道位置发生异常和肠系膜附着不全,是一种先天性肠道 畸形[1]。正常发育过程中,整个小肠系膜从肠系膜上动脉出 发处达到右髂窝呈一条斜线与后腹壁固定。中肠衍化为十 二指肠的后 1/3、空肠、回肠、盲肠、阑尾、升结肠和横结肠的 前 2/3,其血供来源于十二指肠上动脉( SMA) 。先天性肠旋 转不良常伴中肠扭转。 肠旋转不良伴中肠扭转的产前超声直接和特异性的征
象为“漩涡征”。“漩涡征”是指以肠系膜上动脉为轴心,肠 腔螺旋样扭转,肠系膜与系膜血管相伴而形成漩涡状团块, 是构成肠旋转不良伴中肠扭转超声表现的病理学基础[2]。 胎儿肠道内不存在气体干扰,漩涡征较新生儿更易显示。 Shimanuki 等[3]发现,顺时针方向的“漩涡征”对肠扭转的特 异性约 100%,但在常规胎儿腹部横切面难以显示完整的 “漩涡征”图像,因此发现胎儿部分肠管扩张时,应观察是否 存在“漩涡征”。
除特异征象外,还可表现为间接和非特异性征象,如肠 管扩张、腹水、假性囊肿、腹部包块及羊水过多[4]。当扩张的 肠管内壁水肿增厚相互靠拢形成双层厚壁,而外壁较薄,可 出现“咖啡豆征”样改变[5]。胎粪性腹膜炎伴发的腹腔积液 在吸收过程中形成多房囊性表现,形成“假性囊肿”。当无典 型“漩涡征”征象,需与胃肠道重复畸形、梅克尔憩室、节段性 小肠扩张、囊性包块( 畸胎瘤、淋巴管瘤和肠系膜囊肿) 以及 无扭转的肠闭锁和囊性胎粪性腹膜炎等相鉴别[6]。 肠扭转最常见并发症为肠缺血坏死并继发肠穿孔,新生 儿出现拒食、呕吐及腹胀情况。当诊断胎儿肠道扭转后,不 一定需要立即手术,依据孕周,建议在小儿外科的指导下,每 1~3 周复查超声,如胎儿腹部情况恶化,超声每周1~2 次,直 到分娩。胎儿出现腹水及肠蠕动消失时,建议终止妊娠。临 床上对于以呕吐为主要症状且含胆汁或伴消化道出血的新 生儿,腹部平片提示“双泡征”,腹部彩超见“漩涡征”时应高 度怀疑肠旋转不良,消化道造影更适用于诊断婴儿患者是否 有梗阻性病变。
参考文献略。
原始出处:
李 琪,吴海芳,陶国伟等,产前超声诊断肠旋转不良伴中肠扭转 1 例[J],现代妇产科进展,2019,28(12):957-958.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#产前超声#
29
好
73
#产前#
52
#超声诊断#
20
#超声诊断#
24
590kg?
66