Cancer Cell:被忽视的血小板,被发现还可介导抗肿瘤免疫
2022-09-09 生物世界 生物世界
该研究结果表明血小板在 NAFLD 的情况下通过 P2Y12 受体依赖性 CD40L 释放发挥抗肿瘤效力。这些发现是对血小板促肿瘤功能的重要补充,阐明了血小板在肿瘤调节中的复杂作用,并为临床转化提供了
如今,随着不健康的生活方式越来越普遍,非酒精性脂肪肝病已成为全球范围内最常见的肝脏疾病,它与肥胖和2型糖尿病密切相关。
非酒精性脂肪性肝病(NAFLD)以肝脏脂肪堆积为特点,并伴有炎症和胰岛素抵抗。大量被诊断为 NAFLD 的患者进一步会发展为严重形式的非酒精性脂肪性肝炎(NASH),而 NAFLD 和 NASH 都是肝细胞癌(HCC)的重要风险因素。肝细胞癌是肝癌的主要组织学亚型,占原发性肝癌的90%。近几年,肝癌死亡率逐步攀升,在2020年全球癌症发病率中排名第六,在癌症死亡人数排行中排名第三。
在临床研究中,NAFLD 患者通常表现出平均血小板体积增加(血小板数量减少),这是血小板更新的标志物;此外,肝细胞癌患者也经常出现血小板计数或功能异常。这意味着,血小板在常见肝病和肝癌中都发挥了作用。
此前的动物模型研究显示,血小板被激活后在肝脏聚集,从而促进 NASH 发展并驱动随后的肝细胞癌。然而,目前还没有临床研究调查抗血小板治疗对同样具有肝细胞癌风险的 NAFLD 患者的影响。
2022年9月1日,美国国立卫生研究院国家癌症研究所癌症研究中心 Tim Greten 领导的研究团队在 Cell 子刊 Cancer Cell 上发表了题为:Platelets control liver tumor growth through P2Y12-dependent CD40L release in NAFLD 的研究论文。
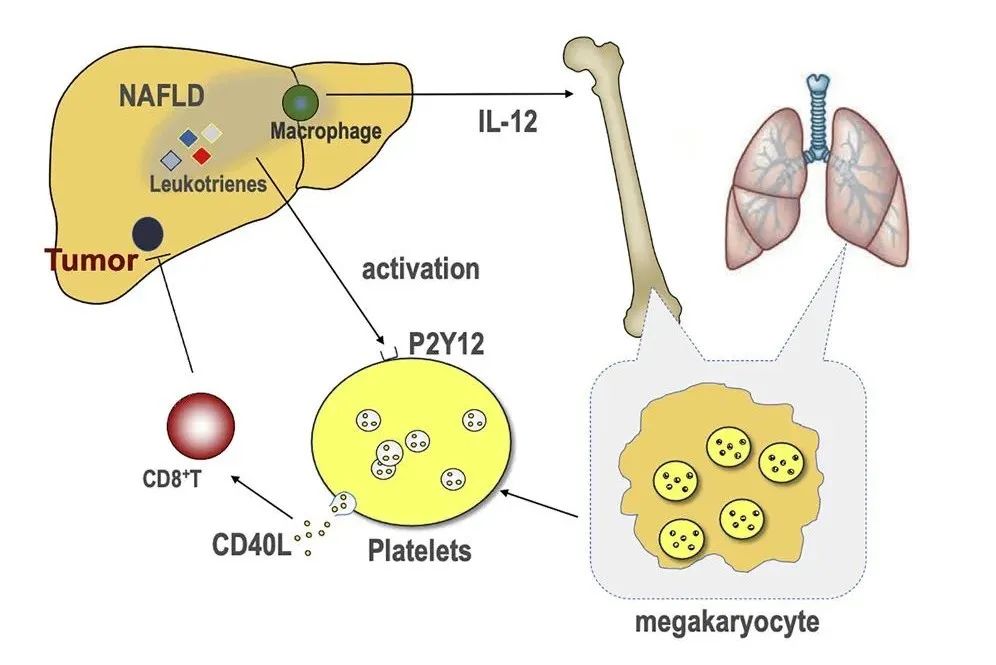
该研究通过在不同品系小鼠、不同饮食 NAFLD 模型和不同的肝细胞癌模型中的研究表明,血小板可以介导抗肿瘤免疫。NAFLD 增加了血小板对 P2Y12 依赖性 CD40L 的释放,从而通过 CD40 和 CD8+T 细胞增强了抗肿瘤免疫。
血小板是从骨髓成熟的巨核细胞胞浆裂解脱落下来的小块胞质,是血液中的一种有形成分。除了作为血栓形成和止血调节剂这种众所周知的功能以外,血小板也是免疫系统的重要组成部分,参与先天性和适应性免疫反应。
最近的临床研究表明,血小板抑制剂阿司匹林降低了病毒性肝炎患者肝细胞癌的风险;抗血小板治疗通过抑制乙型肝炎病毒(HBV)特异性细胞毒性CD8+ T细胞免疫介导的肝损伤,降低慢性 HBV 小鼠模型中的肝细胞癌风险。然而,没有观察到相同的疗法对降低肝细胞癌(HCC)风险的影响。这表明血小板在肝细胞癌中发挥着复杂的作用。
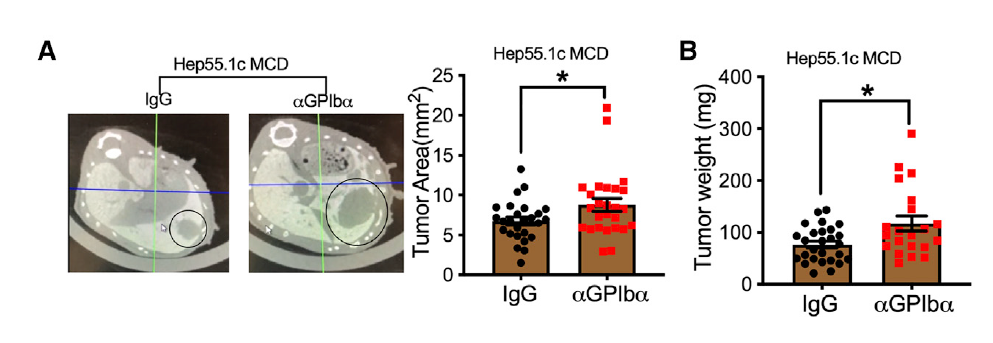
为了研究在 NAFLD 中血小板是否可以调节肝细胞癌的生长,在这项新研究中,研究人员将小鼠原位肝细胞癌肿瘤细胞注射到喂食缺乏蛋氨酸-胆碱饮食的小鼠中。然后用靶向血小板膜糖蛋白Ibα的抗体治疗小鼠,以耗尽荷瘤小鼠的血小板。肿瘤植入后,每 3 天给小鼠腹膜内注射 50μg α-GPIb 抗体或 IgG 对照。7天后,研究人员测量了肿瘤生长情况,并在第21天时测量了小鼠的体重。出乎意料的是,他们发现血小板减少促进了 NAFLD 小鼠肝肿瘤的生长。
为了确认这一发现,研究人员随后反复使用一种抑制血小板聚集的药物氯吡格雷(Clopidogrel,P2Y12受体拮抗剂)证实,该药物治疗增加了 NAFLD 小鼠原位肿瘤的生长。
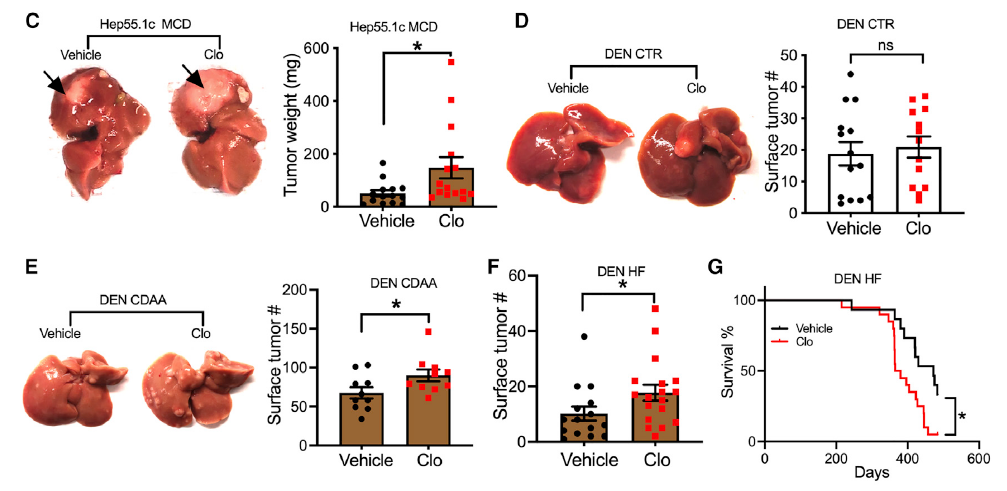
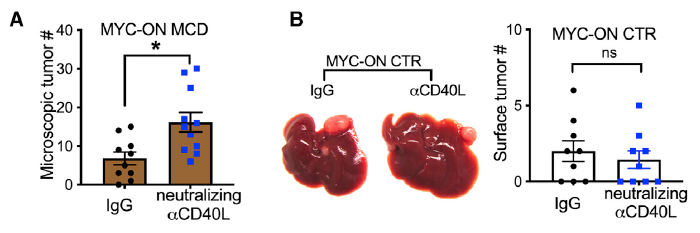
随后,该团队将这一发现扩展到已建立的肝细胞癌肿瘤,致癌物二乙基亚硝胺(DEN)或 MYC 癌基因驱动的多种小鼠肝细胞癌模型中,证实血小板可以抑制 NAFLD 小鼠的肝细胞癌生长;而且他们发现血小板在控制肿瘤生长方面的作用比先前认为的要复杂得多。在 NAFLD 合并肝细胞癌的情况下,血小板既可以通过驱动 NASH 病理表现出促肝癌发生的功能,也可以通过驱动 CD8+T 细胞反应表现出对已建立肿瘤的抗肿瘤活性。
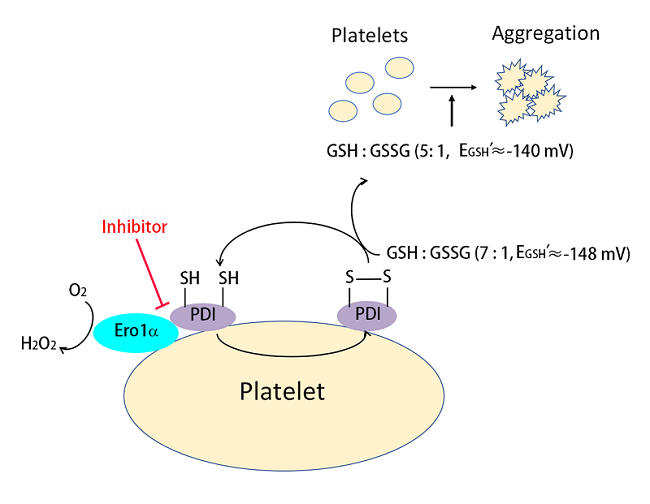
由于血小板是循环 CD40L 的主要来源,血小板衍生的 CD40L 被认为具有功能性且可以调节适应性免疫反应。因此,该团队研究了血小板来源的 CD40L 在肿瘤监测中的作用。
在 NAFLD 小鼠模型和 NASH 患者中,研究人员观察到更高水平的血浆 CD40L;而且,即使在没有肥胖的情况下,NAFLD 也足以增加 CD40L 水平。利用中和抗体和 CD40L 基因缺陷小鼠的进一步研究表明,CD40L 在 NAFLD 肝细胞癌中具有显著的抗肿瘤功能。使用 P2Y12 基因缺陷小鼠证实 P2Y12 在 NAFLD 诱导 CD40L 释放中发挥了关键作用。
此外,该团队通过一项具有挑战性的血小板输注实验,提供了血小板衍生 CD40L 在 NAFLD 模型中具有抗肿瘤功能的直接体内证据。
除了增强 CD40L 释放外,该团队还证明巨噬细胞导致骨髓巨核细胞产生的肝脏 IL-12 和 CD40L 增加。这意味着, NAFLD 中肝脏和骨髓之间存在交叉联系。他们还发现肺巨核细胞在 NAFLD 小鼠中产生更高水平的 CD40L,这表明,肺也可能通过调节 NAFLD 中的血小板来调节肝脏肿瘤。
该团队表示,作为无核细胞片段,血小板拥有功能性剪接体,并通过信号依赖性剪接从前体mRNA生成成熟的信息用于蛋白质翻译,从而形成独特的功能调节机制。由于这项研究仅分析了 CD40L 蛋白,没有测量血小板 CD154 mRNA。因此,不能排除血小板蛋白翻译是否也有助于 NAFLD 中血小板衍生的 CD40L 水平增加。
总之,该研究结果表明血小板在 NAFLD 的情况下通过 P2Y12 受体依赖性 CD40L 释放发挥抗肿瘤效力。这些发现是对血小板促肿瘤功能的重要补充,阐明了血小板在肿瘤调节中的复杂作用,并为临床转化提供了潜在的治疗方法。
论文链接:
https://doi.org/10.1016/j.ccell.2022.08.004
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
92
#cancer cell#
44
在部分HCC中也观察到血小板增多,是否意味着肝癌对于血小板产生调控或是延长了血小板的寿命
23
#Cell#
44
原来血小板也如此神通
47
#血小板#,被发现还可介导抗#肿瘤免疫#
72