BMJ子刊:低血糖与心律失常有关系吗?
2022-01-07 MedSci原创 MedSci原创
研究表明心律失常在接受胰岛素治疗的2型糖尿病患者中很常见,并且与血糖变异性相关,而心律失常与低血糖没有密切关系。
用胰岛素治疗2型糖尿病(T2D)存在诱发低血糖的风险,与患者心血管疾病和死亡风险增加有关。1991年有研究首次报道低血糖期间患者心律失常的风险增加,此后相关的研究层出不穷,这些实验室诱发的低血糖研究几乎一致认为低血糖与心脏复极化异常有关,这也是室性心律失常风险的一个重要标志。
然而,在现实生活中,通过4-5天连续血糖监测(CGM)并同时进行Holter监测的前瞻性观察性研究中,低血糖与临床相关心律失常之间的关联仅提供了很少的证据。因此,有必要对高危2型糖尿病患者进行长期监测研究,以提高对低血糖与心律失常之间关系的认识。
共有21名接受胰岛素治疗的T2D患者(N=21,[平均±SD]年龄66.8±9.6岁,BMI 30.1±4.5 kg/m2,糖化血红蛋白6.8±0.4%[51.0±4.8 mmol/mol])纳入本项为期一年的观察性研究。研究期间,患者接受持续血糖监测([mean±SD] 118±6天)和植入式心脏监护仪(ICM)。
结果显示夜间发生低血糖的时间高于白天。在12名(57%)参与者中检测到724例具有潜在临床意义的心律失常,其中房颤和短暂停搏占发作的99%。日间低血糖与心律失常之间无关联。在夜间,受试者特定的每小时心律失常发生率随低血糖的发生而增加(发生率比[IRR] 1.70 [95% CI 0.36-8.01]),但仅随低血糖时间的增加而略有增加(IRR 1.04 [95% CI 0.89-1.22] / 5分钟)。根据变异系数估计,受试者特定的心律失常发生率在夜间随血糖变异性的增加而增加,而在白天则下降。

白天和夜间低血糖发作的特征
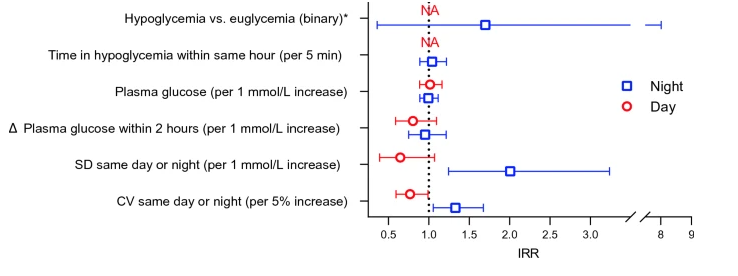
低血糖、血糖变异性和心律失常风险。请注意,在白天低血糖期间未检测到心律失常
总而言之,研究表明心律失常在接受胰岛素治疗的2型糖尿病患者中很常见,并且与血糖变异性相关,而心律失常与低血糖没有密切关系。
参考文献:Andersen, A., Bagger, J.I., Sørensen, S.K. et al. Associations of hypoglycemia, glycemic variability and risk of cardiac arrhythmias in insulin-treated patients with type 2 diabetes: a prospective, observational study. Cardiovasc Diabetol 20, 241 (2021). https://doi.org/10.1186/s12933-021-01425-0
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#BMJ#
32
学习了
53
学习了,谢谢分享
45