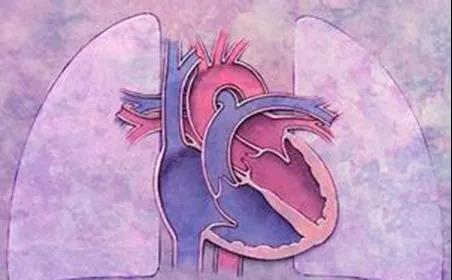
面对妊娠合并肺动脉高压,产科医生能做什么?
2019-05-21 妇儿君 妇儿中心
严重的肺动脉高压和长期的低氧血症还可致胎儿宫内缺氧,导致流产、早产、胎儿窘迫和胎儿生长受限,低体重儿和早产儿呼吸窘迫综合征发生率明显增加,围生儿病死率和死亡率显着增加。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#动脉高压#
27
#产科医生#
33
当时看人世间就觉得这个女的太犟了
77
案例给予的警示
88
学习学习学习
56
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
48