JTO:低剂量CT在非吸烟者肺癌筛查中的意义
2018-11-18 肿瘤资讯编辑部 肿瘤资讯
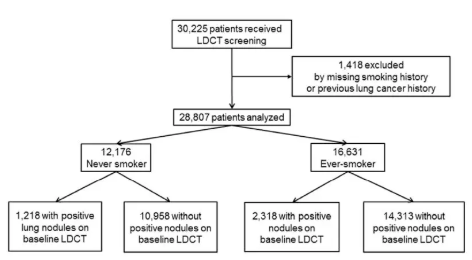
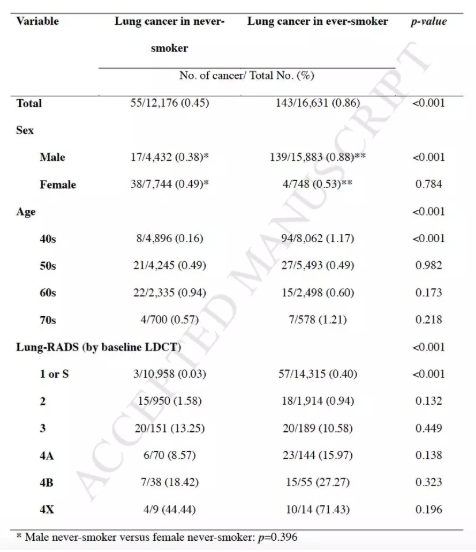
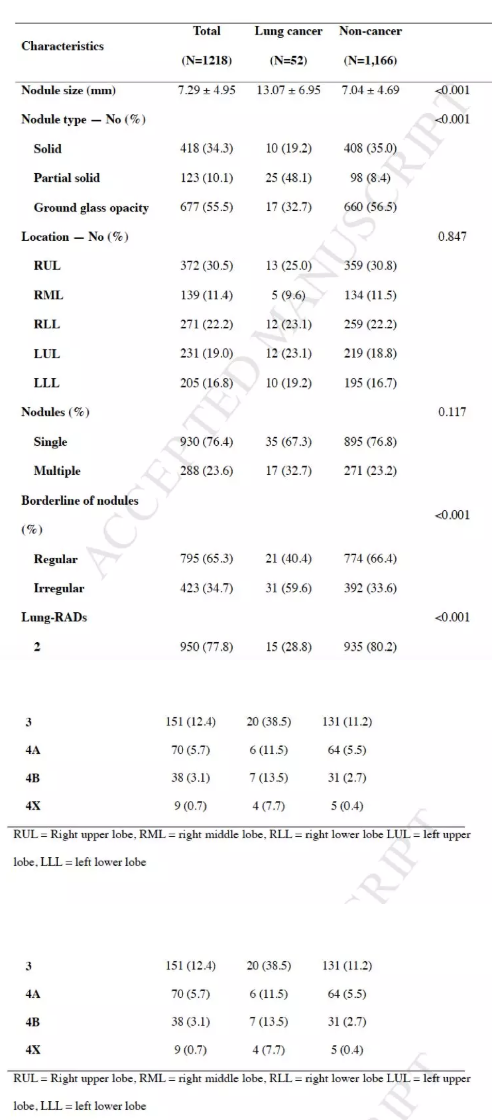
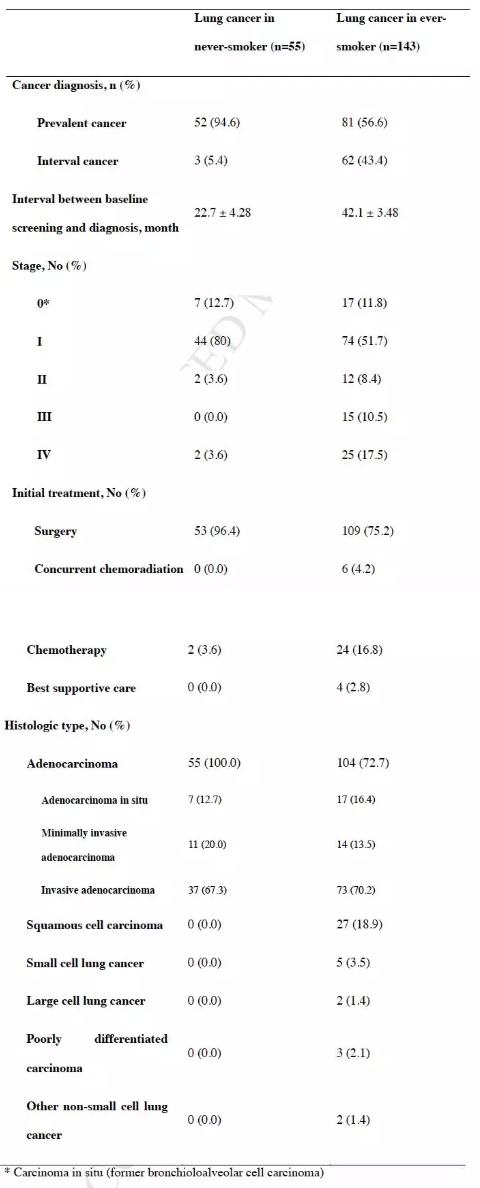
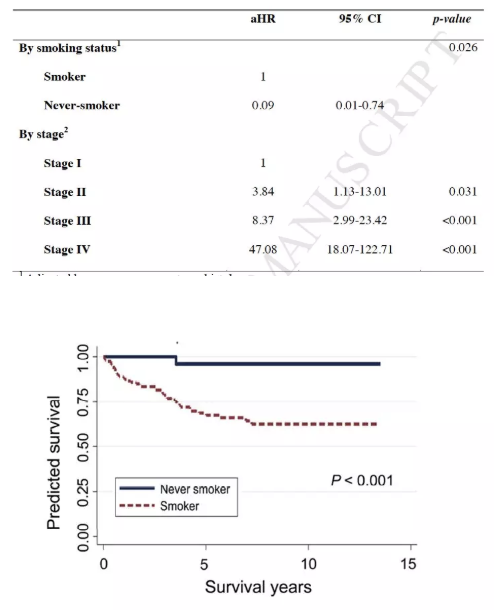
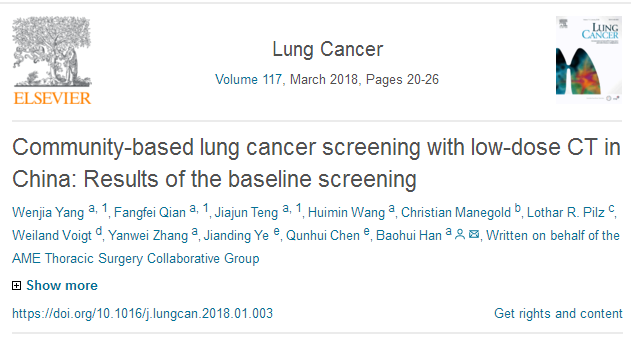
NLST研究和NELSON研究的阳性结果,支持采用低剂量CT对吸烟者进行筛查,未来的研究应该考虑在非吸烟者进行低剂量CT筛查。近年来,非吸烟腺癌患者逐年增长,那么低剂量CT筛查在非吸烟人群中的意义如何?近日发布在JTO杂志的一项研究回顾性分析了低剂量CT在非吸烟者肺癌筛查中的意义。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JTO#点击进入话题查看更多相关文章 或评论时插入话题加入讨论
70
#低剂量CT#
40
#低剂量#
28
#吸烟者#
38
学习了,谢谢分享
69
谢谢了,学习
64
学习了很有用不错
49