近日,耶鲁大学癌症中心研究团队在 Nature Medicine 上发表题为“Toward personalized treatment approaches for non-small-cell lung cancer”的研究文章,对非小细胞肺癌的研究进展进行了总结与展望,研究介绍了目前为 NSCLC 开发的突破性疗法和联合疗法,并强调了新辅助疗法和维持治疗在治愈早期肺癌方面的重要性。
一、肺癌及治疗现状
该项研究指出,肺癌作为导致癌症患者死亡的最主要病因,预计在2021年,将使全球死亡人数超过180万。而在肺癌中,85%属于亚型非小细胞肺癌(non-small-cell lung cancer,NSCLC),在过去十年中,针对NSCLC的治疗模式发生了巨大变化,这主要得益于靶向与免疫疗法的发展。
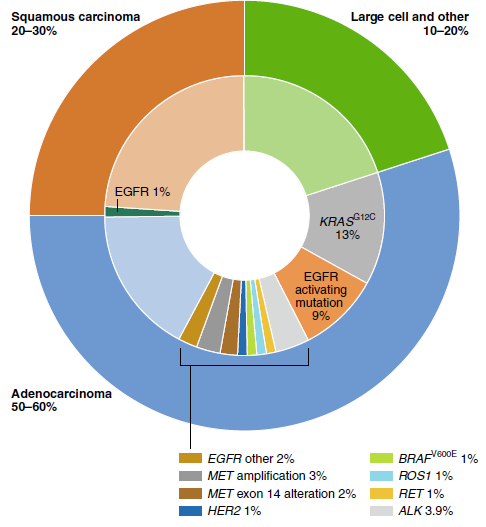
非小细胞肺癌分子突变图谱
自2001年第一次针对表皮生长因子受体(EGFR)的试验开展以来,靶向疗法正改变着肺癌治疗方案。如今,针对EGFR、ALK、RET、BRAF、ROS1、NTRK、MET和KRAS等靶点的抑制剂已经收获了显着成效,其中许多已经成为了一部分患者的标准治疗药物。但值得注意的是,只有不到25%的患者能从靶向治疗中获益,而这些患者在治疗过程中产生耐药性几乎成为必然。
对于表现为EGFR或ALK突变的晚期非小细胞肺癌患者而言,十年前的平均生存期不到2年,而如今,使用第二代和下一代EGFR或ALK抑制剂,中位生存期分别超过3年和5年。
对于大多数没有明确靶向疗法选择的非小细胞肺癌患者来说,联合化疗方案在40多年来一直是主流,只不过在这一疗法下,晚期或转移性癌症的中位总生存期(OS)不到2年。免疫化疗联合疗法现在广泛应用于晚期或转移性NSCLC患者,这些患者基本没有EGFR、ALK或其他驱动因子变异。尽管取得了一些进展,但不幸的是,转移性NSCLC患者的中位总生存期仍不到3年。
二、免疫治疗联合疗法
目前,有大量早期临床研究报告了免疫疗法间的联合应用,包括替代ICB、激动剂共刺激细胞因子或受体、溶瘤病毒以及癌症疫苗等疗法。其中,靶向CTLA-4与抗PD-1/抗PD-L1治疗相结合、TIGIT与抗PD-1/抗PD-L1治疗相结合的组合疗法颇具应用前景。
同时阻断CTLA-4和PD-1共抑制信号通路的免疫联合疗法在临床前研究中显示可以起到互补作用,可用于治疗黑色素瘤、肾细胞癌和非小细胞肺癌患者。对晚期非小细胞肺癌患者进行的两项研究表明,与单纯化疗相比,在抗PD-1治疗中加入抗CTLA-4疗法可提高患者的生存率。
同时阻断TIGIT和PD-1/PD-L1通路可增强肿瘤抗原特异性CD8+T细胞的扩增和功能。目前有研究显示,在那些含有高PD-L1的肿瘤中,TIGIT联合治疗取得了更为深远的改善。
但是总体来说,免疫治疗联合研究的1期和2期数据并不理想,与免疫化疗组合相比,还没有随机试验显示免疫治疗联合疗法有显着改善。对协同作用机制的理解有限、最佳治疗计划布局、最佳治疗持续时间以及如何最好地解决获得性耐药问题,成为了免疫治疗联合疗法的重大挑战。
三、靶向疗法与精准免疫疗法相结合
目前,抗VEGF药物已被证明具有免疫调节作用,因此,针对肿瘤血管系统的靶向疗法与免疫疗法相结合将成为一种合理的组合方法。同时,小分子靶向VEGF(VEGFRs)受体也有可能增强免疫疗法的活性,或提升肿瘤对免疫疗法的敏感度。初步2期数据表明,VEGFR抑制剂-免疫疗法组合在NSCLC患者中具有良好的抗肿瘤活性,但仍然需要随机临床试验数据作为更有力的支撑。

靶向疗法和免疫化疗的总生存期图解,图a为靶向疗法,图b为免疫化疗疗法
除了针对晚期NSCLC患者进行治疗,该项研究提到,约50%的早期(仅局限于局部疾病)NSCLC患者存活期将无法超过5年,这为改善预后留下了充足的空间,因此,将最有效的治疗方法应用于早期和可治愈的患者一直是肺癌治疗的策略。
事实上,最近的数据表明,在辅助/新辅助治疗以及维持治疗环境下,靶向治疗和免疫治疗具有显着益处,支持早期干预。诸多2期研究探索了新辅助免疫治疗方案,这些初步数据表明,免疫化疗有可能改善长期临床结果,包括治愈一些早期非小细胞肺癌患者。
该研究同样提到,对早期肺癌的研究应该以治愈为目标,进一步探索各种组合方法。例如,对于含有高生物标志物的肿瘤,可致力于研究新辅助免疫化疗与手术或放疗相结合的疗法;针对致癌基因驱动的肿瘤,可探究新辅助分子靶向疗法与术后治疗相结合的组合;对于KRAS-G12C突变型NSCLC,使用免疫疗法和KRAS-G12C抑制剂的组合方法可能会在早期疾病治疗中产生更好的结果。
过去十年,转化研究和临床研究改变了非小细胞肺癌的检测与治疗管理,事实上,非小细胞肺癌死亡率正在以每年2%以上的速度下降,这一结果将会持续改善。但同时,未来十年也面临重大挑战,想要成功开发合理的组合疗法,以最大限度根除肿瘤,一个主要挑战将是应用强大的预测生物标志物为每位患者制定个性化的明确策略,让我们期待未来十年非小细胞肺癌治疗领域的更多重大进展!
原始出处:
Wang, M., Herbst, R.S. & Boshoff, C. Toward personalized treatment approaches for non-small-cell lung cancer. Nat Med 27, 1345–1356 (2021). https://doi.org/10.1038/s41591-021-01450-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CIN#
26
#Nat#
31
#DIC#
24
#非小细胞#
24
#Medicine#
37
#Med#
19
话题很赞
45