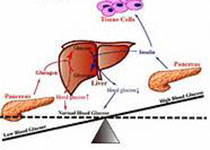
Diabetic Med:糖尿病相关的下肢截肢发病率与糖尿病足护理密切相关,且随着护理的提高而改善
2018-03-25 MedSci MedSci原创
近日,国际杂志 《Diabetic Med》上在线发表一项关于糖尿病有关的主要下肢截肢发病率与糖尿病足护理密切相关,并随着护理的提高而改善的同行评议的研究。该研究调查英格兰西南地区糖尿病相关的下肢截肢发生率与足部护理的关系。 研究于英格兰在西南某一地区引入10项足部护理服务,从2007年开始,该区域足部溃疡发病率稳定,截肢发病率持续下降。引入的服务包括行政支持,标准化普通足部筛查,改善社区足
近日,国际杂志 《Diabetic Med》上在线发表一项关于糖尿病有关的主要下肢截肢发病率与糖尿病足护理密切相关,并随着护理的提高而改善的同行评议的研究。该研究调查英格兰西南地区糖尿病相关的下肢截肢发生率与足部护理的关系。 研究于英格兰在西南某一地区引入10项足部护理服务,从2007年开始,该区域足部溃疡发病率稳定,截肢发病率持续下降。引入的服务包括行政支持,标准化普通足部筛查,改善社区足病护理人员配备,医院多学科诊疗,有效护理路径,矫形师和审计的可用性。对该地区的糖尿病足部护理服务进行同行评估,以评估这些服务条款的执行情况,并将其与约克郡和亨伯尔公共卫生观察站医院提供的其他地区的主要截肢发病率统计数据进行比较进而提出了改善服务的建议。在2015年对服务供应和截肢发生率的变化进行了评估。 2013年的初步评估显示,糖尿病相关的3年截肢发生率与糖尿病足部护理服务的充分提供成负相关(P = 0.0024,调整后的R2 = 0.51)。2015年的重复评估发现,六名糖尿病足部护理员报告了两项或两项以上的足部护理服务改善,且结果有所改善。主要截肢发生率和服务提供之间的负相关关系在2012-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
34
#Diabetic#
26
#发病率#
30
#DIA#
28
#截肢#
39
#Med#
29