European Radiology:静音MRA为脑动静脉畸形的评估提供了新的指标
2022-01-19 shaosai MedSci原创
脑动静脉畸形(BAVM)是一种常见脑血管发育畸形,表现为动脉与静脉之间无毛细血管网而直接相连。BAVM的主要治疗方式包括手术、外科和血管内治疗。
脑动静脉畸形(BAVM)是一种常见脑血管发育畸形,表现为动脉与静脉之间无毛细血管网而直接相连。BAVM的主要治疗方式包括手术、外科和血管内治疗。以往的研究表明,带有高流量动静脉(A-V)分流的BAVM与围手术期出血事件的增加和不完全闭塞的风险较高有关。因此在手术切前,对BAVM的高流量A-V分流进行准确识别和定向栓塞是血管内治疗的关键。
数字减影血管造影(DSA)由于其高空间和时间分辨率,是评估高流量A-V分流的金标准。然而,DSA是一种侵入性检查,具有不可避免的手术相关并发症的风险,因此不适用于连续的后续检查。
静音MR血管成像是一种基于动脉自旋标记(ASL)和ZTE技术的新兴成像方法。一些研究报告称,与TOF MR血管成像相比,静音MRA在描绘BAVM的病灶和引流静脉方面较果更佳。
近日,发表在European Radiology杂志的一项研究探讨了静音MRA计算的引流静脉强度(SI)比值与DSA测量的动静脉转运时间之间的关系,以及静音MRA上具有最大rSI的引流静脉的特征与出血表现之间的关系,为BAVM高流量A-V分流提供有价值的影像学参考指标。
本研究对46名接受静音MRA和DSA的BAVM患者(平均年龄33.2±16.9岁)的81条引流静脉进行了回顾性评估。研究了静音MRA上引流静脉的rSI与DSA上A-V转运时间之间的相关性。同时生成AUC-ROC以评估rSI在确定是否存在高流量A-V分流的性能。进一步比较了出血性和非出血性未经治疗的BAVM之间具有最大rSI(rSImax)的引流静脉的特征。
静音MRA上各引流静脉的rSI与DSA的A-V转运时间明显相关(r = -0.81,p < .001)。使用rSI确定高流量A-V分流的AUC-ROC为0.89。rSI的临界值为1.09,其敏感性为82.4%,特异性为82.8%。出血组的引流静脉具有rSImax且没有异位的情况明显更多(P = 0.045)。
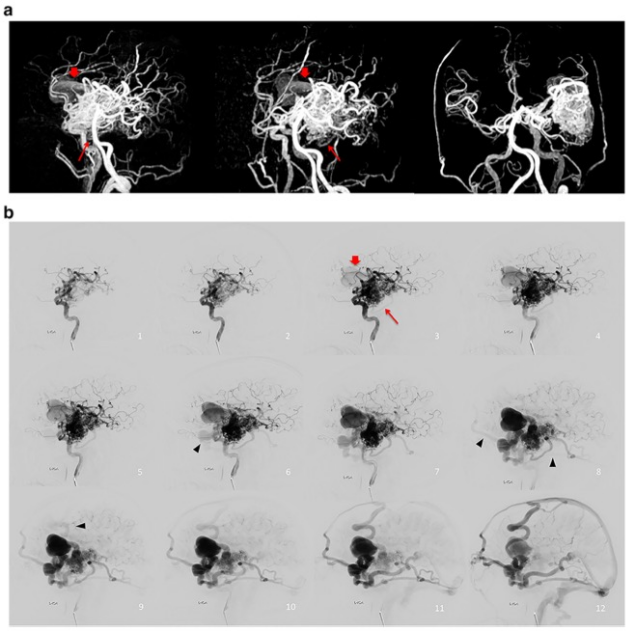
图 64岁男性,左颞部BAVM的图像,有几条的引流静脉向上矢状窦、乙状窦和直窦方向延伸。 a 静音MR血管造影的三维MIP显示一条扩张的引流静脉(红色箭头)和一条小的引流静脉(红色长箭头)。请注意,在DSA上描绘出病灶后四帧以上观察到的几条引流静脉(黑色箭头),在静音MRA上是看不到的。
本研究表明,静音MRA测量的引流静脉SI比率与DSA上BAVM的动静脉转运时间具有相关性。静音MRA上的rSI可作为评估BAVM高流量A-V分流的潜在影像学标志物。
原文出处:
Chun-Xue Wu,Zhen-Xiang Zang,Tao Hong,et al.Signal intensity ratio of draining vein on silent MR angiography as an indicator of high-flow arteriovenous shunt in brain arteriovenous malformation.DOI:10.1007/s00330-021-08170-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
36
#静脉#
47
#动静脉畸形#
55
学习
67
#畸形#
47
#MRA#
46