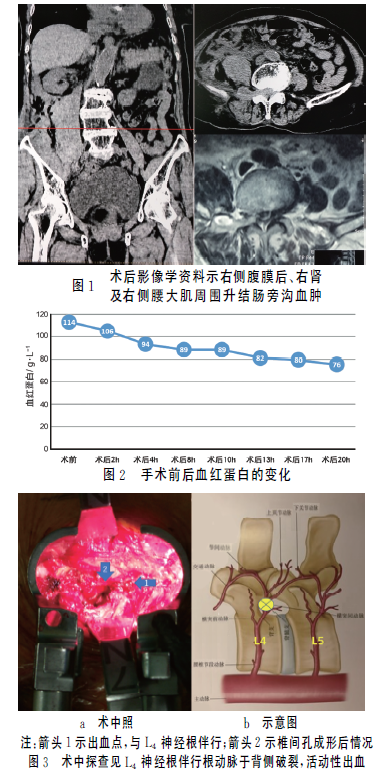
腹膜后多器官累及的黄色肉芽肿1例
2018-11-26 张红伟 吕发金 中国医学影像学杂志
女,58岁,因“肛门坠胀8个月余,加重半个月”入院,伴大便次数增多,每日排稀便10余次,量少,无腹痛、腹胀,无尿频、尿急等不适,经治疗症状可减轻,但反复发作。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#腹膜后#
27
很好的学习机会
55
#肉芽肿#
26
#腹膜#
34
了解一下,谢谢分享!
74