J Gastroenterology H:氨甲环酸对结肠憩室出血患者的影响
2021-06-03 MedSci原创 MedSci原创
结肠憩室出血是成人下消化道出血的主要原因,虽然有70-90%的结肠憩室患者出血会自己停止,然而,在一些严重的情况下,它可能导致严重的消化道出血。
结肠憩室出血是成人下消化道出血的主要原因,虽然有70-90%的结肠憩室患者出血会自己停止,然而,在一些严重的情况下,它可能导致严重的消化道出血,有时需要内镜止血、动脉栓塞或结肠切除术,在最严重的情况下,可能会导致患者的死亡。氨甲环酸 (TXA)是氨基酸赖氨酸的合成衍生物,可竞争性抑制纤溶酶原激活为纤溶酶并直接抑制纤溶酶激活。因此,它可作为纤维蛋白溶解抑制剂,防止血栓分解和减少出血。以前的多中心试验表明,TXA 可降低外伤性出血、手术出血和产后出血患者的死亡率。然而,TXA 对结肠憩室出血患者的影响仍不清楚,因此,本项研究旨在探究 TXA 对结肠憩室出血患者的疗效。

研究人员在日本进行了一项全国观察性研究,纳入了 2010 年至 2018 年间因憩室出血入院的患者。患者入院当天接受 TXA 的患者为 TXA 组,其余患者为对照组。主要结局是院内死亡率。次要结局包括严重出血、入院 7 天内输血、住院时间和住院费用。
最后共有78 291 名患者本项研究的纳排标准,并且通过一对一的倾向评分匹配创建了 30 526 对配对队列。匹配后,两组住院死亡率无显着差异([OR],1.07;95%[CI],0.88-1.30);然而,TXA 给药与严重出血事件(OR,0.93;95% CI,0.89–0.99)、输血(OR,0.88;95% CI,0.84–0.92)、住院时间缩短(差异, -0.23 天;95% CI,-0.01- -0.44 天),以及较低的总住院费用(95% CI,-$153 - -$314)有关。
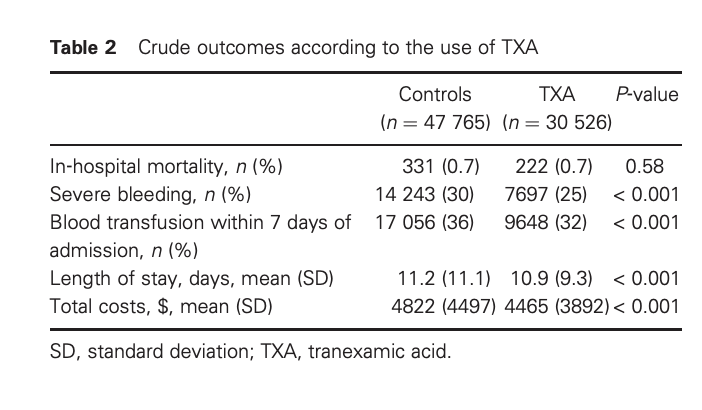
图:氨甲环酸对于各种并发症的影响
研究人员最后说道:尽管 TXA 与较低的住院死亡率没有显着相关性,但它可能会减少严重出血、输血、住院时间和住院费用,因此,临床中应重视TXA的使用指征。
原始出处:
Yuki Miyamoto. Et al. Effect of tranexamic acid in patients with colonic diverticular bleeding: A nationwide inpatient database study. Journal of Gastroenterology and Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AST#
42
#GAS#
38
#Gastroenterol#
37
手上恰好有这类患者,值得一试
84
#Gastroenterology#
45
#憩室#
42
大开眼界,
65
已读,真是受益匪浅呀。
82