粪便预测大肠癌
2015-10-19 佚名 生物谷
根据一项新的调查研究显示,通过分析大肠癌患者病灶附近的微生物组群相比于传统的血液检测有很多的优点:灵敏度与特异性都要更高,而且无创。 “大肠癌患者体内的微生物组群构成一定会有相应的改变,因为不同的基因突变可能会造成不同的癌症类型,这些肿瘤也会对周围的微生物组造成一定的影响”。来自民尼苏达大学的Ran Blekhman博士说到。 该研究结果发表在2015年美国人类遗传协会的会议上。 在该研

根据一项新的调查研究显示,通过分析大肠癌患者病灶附近的微生物组群相比于传统的血液检测有很多的优点:灵敏度与特异性都要更高,而且无创。
“大肠癌患者体内的微生物组群构成一定会有相应的改变,因为不同的基因突变可能会造成不同的癌症类型,这些肿瘤也会对周围的微生物组造成一定的影响”。来自民尼苏达大学的Ran Blekhman博士说到。
该研究结果发表在2015年美国人类遗传协会的会议上。
在该研究中,Blekhman与同事们比较了正常大肠细胞与大肠癌肿瘤细胞间的遗传差异,他们发现特定的肿瘤相关基因突变与特异性的大肠寄生细菌有很大关系。
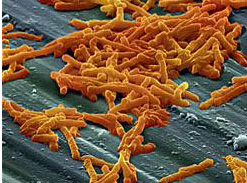
例如,具有APC基因突变的人群易得腺瘤性息肉病(一类遗传性的癌症),同时他们体内肿瘤组织附近具有大量的梭杆菌。Blekhman博士指出他们实验室第一次分析了这种肿瘤相关突变与肿瘤周围微生物组之间的关系。
研究者们通过全基因外显子测序的手段分析了肿瘤组织周围(或者对照正常组织周围)的微生物组的组成。不同的突变往往与特定微生物类型种群丰度有相关性。另外,同一样品内部如果遗传突变越多,其周围鉴定出的微生物种群类型也就越多。
通过突变手段,作者们发现如果肿瘤细胞内葡萄糖转运通路被阻断的话,微生物群所需的能量消耗也就越多。这说明在某些情况下肿瘤与周围的微生物在竞争性地使用体内的资源。
之后,研究者们以微生物的种类与丰度为标准评估了一些肿瘤相关遗传突变。这一结果能够准确预测ZFN717基因的突变。该基因能够编码锌指核酸酶用于DNA的修复。该结果也表明我们可以通过分者粪便中的微生物成分大致预测肿瘤的类型,而且理论上也可以通过控制肿瘤微环境预防、治疗癌症。
原文出处:
推荐原文报道:Microbiome May Predict Colon Cancer Tumor Mutational Status
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
67
赞
113
这也可以?
92
好学习很值得好学习
121
好学习很值得
102
这样好,可以早期筛查
124
有意思
81
研究新进展吗
40
#粪便#
39
肠细菌群器官
73