Blood:血管免疫母细胞性T细胞淋巴瘤的预后和预后因素
2021-08-01 Nebula MedSci原创
一种新的预后评分划分了具有不同临床预后的低、中和高风险 AITL 亚组
中心点| 血管免疫母细胞性 T 细胞淋巴瘤(AITL)的现代治疗方法仍不理想;一种新的预后评分划分了具有不同临床预后的低、中和高风险 AITL 亚组。
血管免疫母细胞性 T 细胞淋巴瘤 (AITL) 是外周 T 细胞淋巴瘤 (PTCL) 的一种独特亚型,具有独特的临床病理特征,侵袭性强,预后差。
在近期发表在《血液》杂志上的一项研究中,Ranjana等对2006年至 2018 年期间参加国际前瞻性 T 细胞项目的282名 AITL 患者进行了亚组分析。主要和次要终点分别是5年总生存期(OS)和无进展生存期(PFS)。研究人员还分析了临床协变量和24个月内病程进展 (POD24) 的预后影响,并开发了一种新的预后评分方法。
整体的OS和PFS
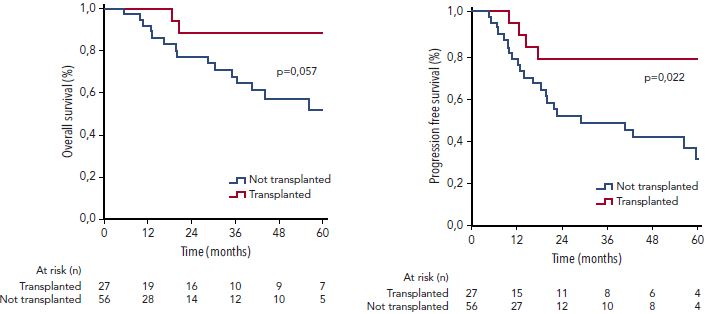
受试患者的中位年龄为64岁,90%的患者为晚期疾病。81%的患者接受了基于蒽环类药物的方案治疗,13%的患者在首次获得完全缓解 (CR1) 时接受了巩固性自体干细胞移植 (ASCT)。5年OS和PFS估计值分别为44%和32%,完全缓解时接受ASCT的患者的临床预后有所改善。
完全缓解时有无ASCT的患者的OS和PFS
在多变量分析中,≥60岁、ECOG表现状态>2、C反应蛋白升高和β2微球蛋白升高都与预后不良相关。结合了上述这些因素的一种新的预后评分(AITL 评分)划分了低、中和高风险亚组,对应的5年OS估计值分别为63%、54%和21%,具有比既定预后指数更大的鉴别力。
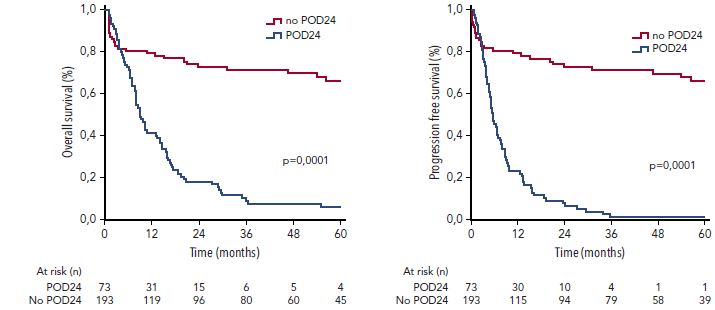
有无POD24的患者的OS和PFS
最后,POD24是一个强有力的预后因素,没有POD24的患者的5年OS高达63%,而有 POD24 的患者的5年OS仅有6%(p<0.0001)。
总而言之,AITL 的最佳治疗仍然是一个未被满足的需求,我们需要探索新的治疗方法。该研究结果需要在前瞻性的队列研究中进一步进行验证。
原始出处:
Ranjana H. Advani, et al. Outcomes and prognostic factors in angioimmunoblastic T-cell lymphoma: final report from the international T-cell Project. Blood (2021) 138 (3): 213–220. https://doi.org/10.1182/blood.2020010387
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#细胞性#
51
学习
46
学习
35
学习
52
#细胞淋巴瘤#
50
#T细胞淋巴瘤#
52
#预后因素#
40