【1】抗坏血酸、皮质类固醇和硫胺素并不能改善感染性休克的器官损伤
为了确定抗坏血酸、皮质类固醇和硫胺素的组合是否能减轻感染性休克患者的器官损伤,研究组进行了一项安慰剂对照、随机、双盲、多中心临床试验。2018年2月9日至2019年10月27日,在美国14个中心共招募了205位感染性休克患者。将其随机分组,其中103例接受静脉外抗坏血酸、氢化可的松和硫胺素治疗,每6小时一次,共4天;102例在同一时间点接受安慰剂治疗。205名患者的平均年龄为68岁,44%为女性,其中200名(98%)至少接受1剂研究药物,完成试验并被纳入分析(干预组101例,安慰剂组99例)。入组后72小时内,干预组的平均SOFA评分从9.1分降至4.4分,安慰剂组则从9.1分降至5.1分,干预前后组间差异均无统计学意义。干预组中肾功能衰竭的发生率为31.7%,安慰剂组为27.3%,组间无显著差异;干预组的30天死亡率为34.7%,安慰剂组为29.3%,亦无显著差异。干预组中最常见的严重不良事件包括12例高血糖症、11例高钠血症和13例新发医院感染;安慰剂组中则分别有7例、7例和12例。总之,抗坏血酸、皮质类固醇和硫胺素的组合治疗感染性休克患者,与安慰剂相比,入组后72小时内并不能显著改善SOFA评分。
【2】糖尿病-抑郁协同干预对共病患者临床症状的改善作用
近日研究人员考察了糖尿病-精神疾病共护理模式,对成年糖尿病伴抑郁症患者抑郁症状和心血管代谢指标的影响。研究在印度开展,招募了2型糖尿病患者,患者健康问卷9评分至少为10分,血红蛋白A1c (HbA1c)至少为8%,收缩压(SBP)至少为140 mm Hg,或低密度脂蛋白(LDL)胆固醇至少为130 mg/dL。随机分为联合干预组(n=196)或对照组(n=208),联合患者接受了非医师护理协调员12个月的自我管理支持,电子健康记录决策支持以方便医生调整治疗和专家病例回顾,随后在无干预的情况下再随访12个月。对照患者接受24个月以上的常规护理。404名患者平均年龄53岁,男性占40.8%,378名患者(93.5%)完成了试验。联合干预组与常规护理组相比,达到主要结果的患者比例显著增加。在16个预先指定的次要结果中,组间在12个月时的10个结果以及24个月时的13个结果间没有统计学上的显著差异。干预组和常规护理组的严重不良事件包括心血管事件或住院、中风、死亡以及严重低血糖。研究认为,对于糖尿病伴抑郁症患者,共病协同干预可显著改善患者24个月时抑郁症状和心血管代谢指标。
【3】患有重症COVID-19的年轻男性中存在基因变异
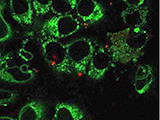
为了探讨年轻COVID-19患者中原发性免疫缺陷与存在基因变异是否有相关性,研究组招募因重症COVID-19而进入重症监护病房(ICU)的年轻(年龄<35岁)、无病史的成对兄弟。2020年3月23日至4月12日,荷兰4家医院的ICU收治了来自2个无关家庭的4名男子。快速临床全外显子组测序结果用于鉴定潜在的单基因病因。随后,在从患者和家属分离的原代免疫细胞中进行了基本的基因和免疫学测试,以鉴定任何免疫缺陷。4例男性患者的平均年龄为26岁(21-32岁),无重大慢性病史。他们在因严重COVID-19而出现呼吸功能不全,需要在ICU中进行机械通气之前,身体状况一直良好。通气支持的平均时间为10天,ICU的平均住院时间为13天。有1名患者死亡。对患者进行快速临床全外显子组测序,并在可用的家族成员中进行分离,确定了TLR7 X染色体功能缺失变体。在家族1的成员中,鉴定出了母亲遗传的4-核苷酸缺失;被感染的家族2成员携带了一个错义变体。在患者的原发性外周血单个核细胞中,通过TLR7激动剂咪喹莫特刺激后IRF7、IFNB1和ISG15的mRNA表达显著降低来测量,下游I型干扰素(IFN)信号转录下调。为响应咪喹莫特的刺激,患者的II型IFN-γ产生亦减少。总之,在4例严重COVID-19的年轻男性患者中,鉴定出了与I型和II型IFN反应受损相关罕见的功能丧失的X染色体TLR7变体。这些初步发现有助于了解COVID-19的发病机理。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







很详细,很赞
64
讲的很详细,很有用,赞一个
70
很有用,很不错,谢谢分享
66
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
34