围术期疼痛的全程管理病例分享_高龄、房颤患者腹腔镜Dixon术麻醉镇痛管理病例
2017-10-26 CMT 中国医学论坛报
患者,男,74岁,体重48 kg,本次主因“ 直肠癌4 程新辅助化疗后3 周”入院,拟行“腹腔镜下直肠癌前切除(Dixon)术”。
中山大学肿瘤防治中心 康世阳
病例简介
病例摘要
患者,男,74岁,体重48 kg,本次主因“ 直肠癌4 程新辅助化疗后3 周”入院,拟行“腹腔镜下直肠癌前切除(Dixon)术”。
麻醉情况
患者入室后予常规生命体征监护,血压144/80 mmHg,心电图提示心房颤动,心率为86~105次/min,患者一般状况良好,给予面罩吸氧(2 L/min),血氧饱和度可维持在99%~100%。随后,予咪达唑仑2 mg、依托咪酯14 mg、顺式阿曲库铵10 mg、羟考酮10 mg依次静推麻醉诱导,待患者自主呼吸消失立即予面罩给氧辅助通气,频率为22 次/min。3 min 后行气管内插管,插管后心率最快升至105次/min,立即予机械通气,吸入七氟烷(1.5%),吸入氧浓度调整为60%,总流量为2 L/min,呼吸频率12 次/min,潮气量450 ml。10 min后患者心率可至63 次/min,血压98/62 mmHg。麻醉诱导完成后,遂行右颈内静脉穿刺置管开放中心静脉并行左桡动脉穿刺置管检测动脉血压。术中复合予瑞芬太尼0.1 μg/(kg·min)、重酒石酸间羟胺0.5 μg/(kg·min)静脉泵注。术毕前30 min予羟考酮5 mg、氟比洛芬酯50 mg、帕洛诺司琼0.25 mg 静推,连接PCIA。术毕15 min 后,患者恢复意识、自主呼吸良好,顺利拔出气管导管,无术后烦躁,安全返回病房。PCIA配方及设定:羟考酮35 mg、氟比洛芬酯200 mg、帕洛诺司琼0.5 mg、右美托咪定100 μg,以生理盐水稀释至100 ml,背景剂量2 ml/h,单次给药剂量2 ml,锁定时间5 min。
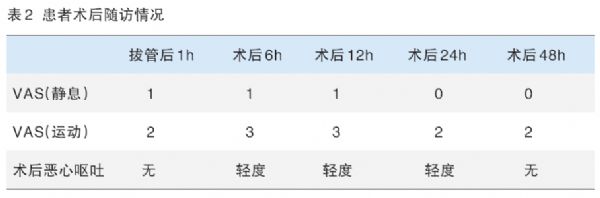
羟考酮总耗量28 mg,患者术后对镇痛效果满意,舒适度良好,VAS评分如表2所示。患者术后第2 天有排气、排便,第4 天可下床活动,无明显呼吸抑制、无过度镇静、无循环系统相关并发症,于术后第5天出院。
腹腔镜手术术后的急性疼痛可造成患者血压升高、心率增快、躁动等一系列并发症,不利于患者术后快速康复,应积极预防和处理。
阿片类药物是目前术后急性疼痛常用的镇痛药物,但是,现有的强阿片类药物(如吗啡、舒芬太尼等)呼吸抑制、镇静作用明显,给术后复苏带来一定的困难。
羟考酮为强效双阿片类受体激动剂(μ和κ受体),主要通过激动κ受体,特别是κ2b受体,因而相比芬太尼(μ受体激动剂),羟考酮对内脏性疼痛有更好的镇痛效果、更轻的呼吸抑制和镇静作用,利于术后患者的苏醒。
本例中,患者高龄且合并房颤,对于围术期血压、心率等循环系统的功能管理十分重要。
手术结束前30 min予羟考酮5 mg 及氟比洛芬酯50 mg 作为镇痛的首量,羟考酮PCIA背景剂量2 ml/h,保证患者在手术后24 h内具有理想的镇痛效果。手术后羟考酮较好的镇痛效果、较轻的呼吸抑制作用,对患者术后的康复有积极意义。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Dixon术#
23
#管理病例#
43
#麻醉镇痛#
42
#围术期#
37
#腹腔镜#
30
#镇痛#
35
#高龄#
30
#全程管理#
31
#房颤患者#
34
学习了受益匪浅
63