BJU Int:一项基于群体的临床显著性前列腺癌筛选随机试验
2022-01-14 AlexYang MedSci原创
评估了使用前列腺特异性抗原(PSA)、激肽释放酶panel和多参数磁共振成像(MRI)进行基于人群筛查试验的可行性,并旨在最大限度地减少过度诊断,同时保留死亡率益处。
癌症筛查的一般原则包括在无症状人群中发现有临床意义的疾病,并有已知的自然进展,早期诊断和治疗可有效改善疗效和降低死亡率。此外,从筛查中获得的益处须大于不良影响,而且筛查必须具有成本效益。

近期,来自芬兰的研究人员在《BJU Int》上发表文章,评估了使用前列腺特异性抗原(PSA)、激肽释放酶panel和多参数磁共振成像(MRI)进行基于人群筛查试验的可行性,并旨在最大限度地减少过度诊断,同时保留死亡率益处。
研究人员从参与度、筛查测试结果和癌症检测方面对筛查算法的可行性进行了评估。他们从人口登记处选择了400名65岁男性的随机样本,并邀请他们进行三个步骤的测试(PSA、激肽释放酶panel和MRI)来进行筛选。那些PSA水平≥3 ng/mL的男性进一步用激肽释放酶panel进行测试,有阳性结果(风险>7.5%)的男性进一步进行前列腺MRI。MRI呈阳性的男性(前列腺成像报告和数据系统[PI-RADS]评分为3-5分)则进行针对性的活检。MRI阴性,但PSA密度≥0.15的男性接受了系统性活检。
受邀的399名男性中,有158人(40%)参与了试验,其中27人的PSA水平≥3纳克/毫升(占被邀请者比例为7%,占参与者比例为17%)。其中,22人的激肽释放酶panel呈阳性(占受邀者比例为6%,占PSA阳性者比例为81%)。最后,有10名男性(占受邀者比例为3%,占激肽释放酶panel呈阳性者比例为45%)有可疑的MRI(PI-RADS评分≥3),5人在融合活检时诊断为有临床意义的前列腺癌(格里森等级组[GG]≥2)(占参与者的比例为3%),有2例GG 1(1%)。因此,在PSA之后进行的附加检测(激肽释放酶panel和MRI)使活检率降低了56%。
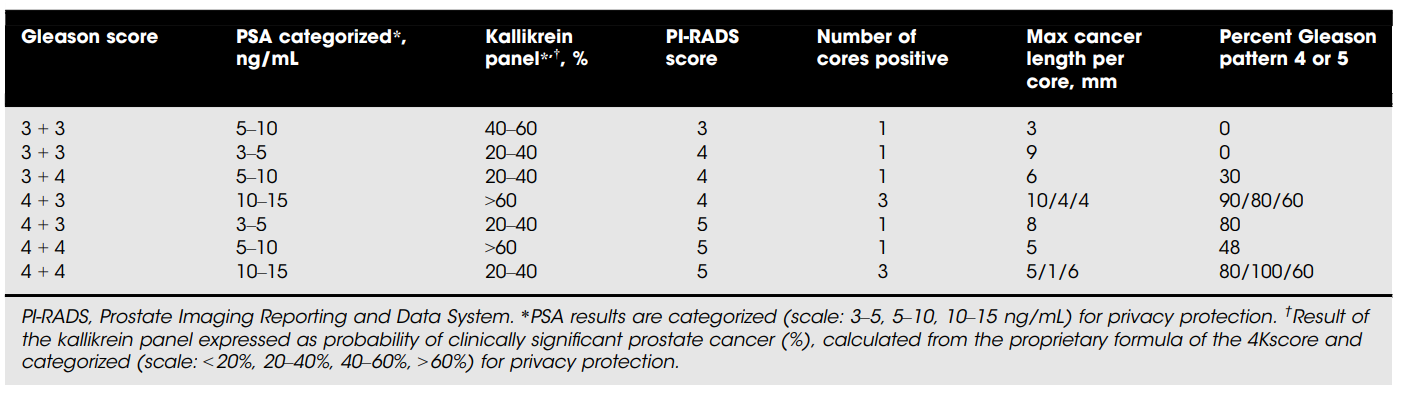
研究中筛选到的患癌男性结果情况
综上所述,他们的结果证明了其筛查方案是有效的,可大幅降低活检比例。然而,参与度情况并不理想。
原始出处:
Antti Rannikko , Mare Leht , Tuomas Mirtti et al. Population-based randomized trial of screening for clinically significant prostate cancer ProScreen: a pilot study. BJU Int. Dec 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#群体#
58
#随机试验#
40
#筛选#
56
随机化
61