Prostate Cancer P D:改善前列腺活检患者风险评估和选择的预测模型研究
2019-04-30 AlexYang MedSci原创
前列腺癌风险预测模型和多参数核磁共振成像(mpMRI)能够用于个性化的活检前风险评估。然而,双参数MRI(bpMRI)已经成为一种更加简单、更加迅速的MRI方法来减少花费并促进其在临床中的应用。bpMRI和风险模型怎样结合起来还是未知。最近,有研究人员基于bpMRI和临床参数为无活检历史的明显前列腺癌(sPCa)患者开发了一个预测模型。研究包括了876名无活检且具有临床疑似前列腺癌的男性(PSA&
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
相关资讯
Prostate Cancer P D:前列腺癌中质子放射治疗与光子放射治疗比较
放射技术的进展改变了局部前列腺癌患者的治疗选择。三维适形放射治疗和可调节强度放射治疗(IMRT)使得医生可以避免邻近正常组织受放射影响,从而减少副作用事件。质子束技术的引入及其在病理组织中能量具有最大范围的物理优势,有可能为前列腺癌患者避免膀胱和直肠等关键器官遭受影响。目前的数据局限于大的和观察性的研究,并且并没有阐释清楚质子治疗比IMRT传统治疗方法的优势。另外,质子束放射治疗的花费也增加了该治
Prostate Cancer P D:转移去势难治性前列腺癌患者中sipuleucel-T单一疗法的PSA稳定性和总生存分析
Sipuleucel-T是一种自体细胞免疫疗法,该疗法获得了FDA的批准用于无症状或者症状微小的转移去势难治性前列腺癌(mCRPC)的治疗。IMPACT注册中心试验阐释了上述疗法的总生存增加了4.1个月,但是在PSA响应或者无进展生存的改善方面结果并不一致。基于一些因素,包括客观治疗的反应,Sipuleucel-T治疗在该类患者群体中规模缩小,尽管当前NCCN推荐使用。最近,有研究人员为了探索是否
Oncogenesis:ZFHX3对ERβ抑制细胞增殖是必不可少的
雌激素受体2(ESR2,也称之为ERβ)和锌指同源框3(ZFHX3,也称之为ATBF1)在小鼠中能够调控前列腺发育和抑制前列腺肿瘤的形成。ZFHX3对ESR1的功能是不可或缺的,ESR1与ESR2属于同一家族蛋白,但是在前列腺上皮中几乎不表达。ZFHX3怎样抑制前列腺致瘤过程仍旧不清楚。最近,有研究人员调查了是否ZFHX3和ERβ在抑制前列腺致瘤过程中存在互作。在C4-2B和LNCaP雄激素受体(
Cancer Res:发现前列腺癌新靶标
前列腺癌是一种泌尿系恶性肿瘤,对中老年男性造成了巨大的危害。通常,前列腺癌发展较为缓慢而易于治疗。去势治疗是治疗前列腺癌的标准治疗方式之一。然而由于去势治疗后发展的抵抗一直缺乏相应的治疗靶点,也是前列腺癌治疗中的瓶颈。其中,大部分的去势抵抗患者最终转变为转移性去势抵抗,而转移是导致前列腺癌患者死亡的主要原因。因此,前列腺癌的侵袭转移成为诊断和治疗的重点研究对象,而独立于雄激素信号通路和去势抵抗的新
J Med Chem:研发出克服前列腺癌临床耐药的新型RORγ抑制剂
在本项工作中,研究团队利用片段组合及基于蛋白结构的优化策略,针对前期获得的前列腺癌新靶标RORγ发展了一种新型抑制剂XY101。该化合物显着抑制RORγ的转录活性(IC50 = 30 nM),具有优越的选择性、良好的代谢稳定性和体内生物利用度(T1/2 = 7.32 h, F = 59%)。在体外,化合物XY101可以抑制多种前列腺癌细胞的增殖与克隆形成,同时可有效抑制前列腺癌细胞中AR、AR-v
Sci Rep:前列腺癌细胞的高通量、时间分别率力学表型分析
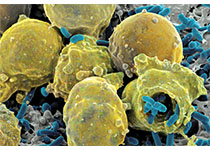
世界范围内,前列腺癌是仅次于肺癌的男性诊断疾病。甚至是最好的诊断标准仍旧缺乏精度,导致组织检测的假阳性从而导致患者接受不必要的外科手术干预。明确的早期诊断工具的缺乏是一个很明显的问题。最近,有研究人员呈现了微流体平台,时间分辨流体力学拉伸器(TR-HS),该设备可以允许每秒内对上千个细胞的非破坏性应力进行动态的力学响应调查。TR-HS整合了高速成像和计算机视觉,从而实现悬浮于液体中单个细胞的自动化













#Prostate Ca#
33
#前列腺活检#
33
#预测模型#
23
#活检#
30
#ROS#
25
#PRO#
23
梅斯里提供了很多疾病的模型计算公式,赞一个!
48