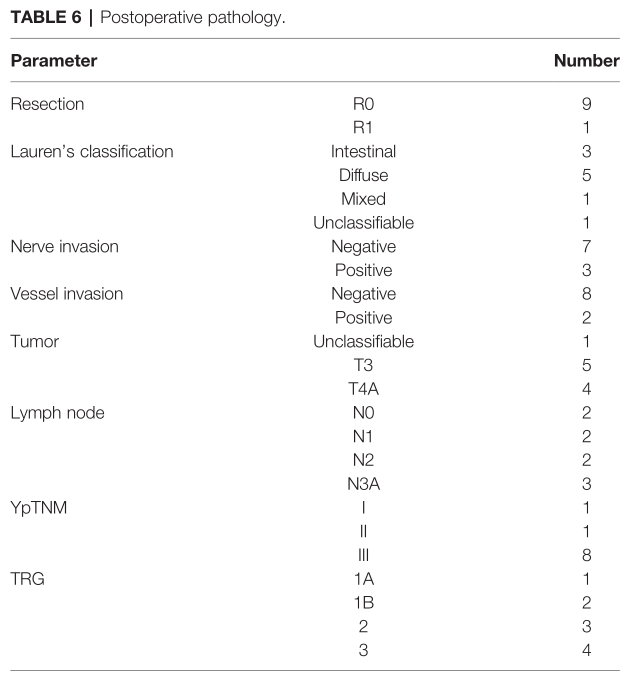
Front Oncol: FOLT方案围手术期治疗中国局部晚期胃癌的可行性和安全性
2021-10-02 yd2015 MedSci原创
研究表明,FLOT方案作为中国局部晚期胃癌新辅助治疗安全有效,辅助治疗的剂量应适当调整。肿瘤病理退缩以及生存需要进一步大样本队列验证。
FLOT方案(氟尿嘧啶加亚叶酸钙、奥沙利铂和多西他赛)作为新辅助对胃癌患者有显著益处。然而,该方案在亚洲国家并没有被很好地接受。因此,来自上海交通大学瑞金医院的团队开展了前瞻性研究,评估FLOT方案在中国局部晚期胃癌患者中的安全性和可行性。相关结果发表在Frontiers in Oncology杂志上。
研究纳入胃或食管胃连接处腺癌患者,接受4周期FLOT方案先辅助化疗,术后再接受4周期FLOT方案辅助化疗。分析化疗完成情况、不良事件、术后发病率和肿瘤病理退缩等情况。评估2年总生存率(OS)和无复发生存率。
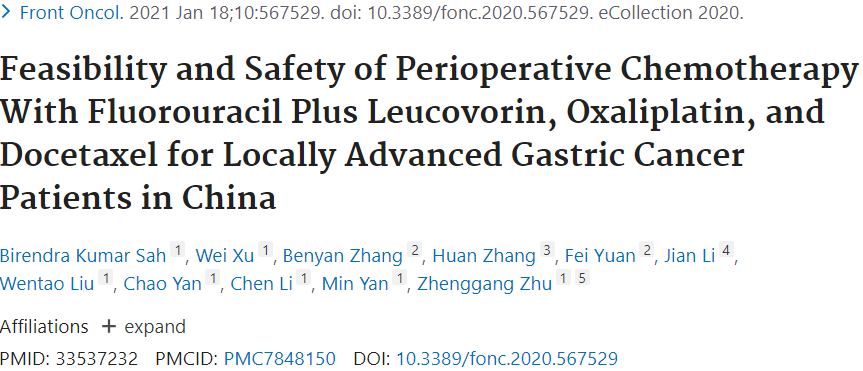
一共纳入10例患者,所有患者均完成4个周期的新辅助化疗。除一例3级贫血外,没有严重的血液学不良事件(3级或以上)。4例患者出现3级或4级呕吐,所有其他非血液学不良事件均为2级或以下。4例患者达到部分缓解(PR),6例患者获得疾病稳定(SD)。
不良事件
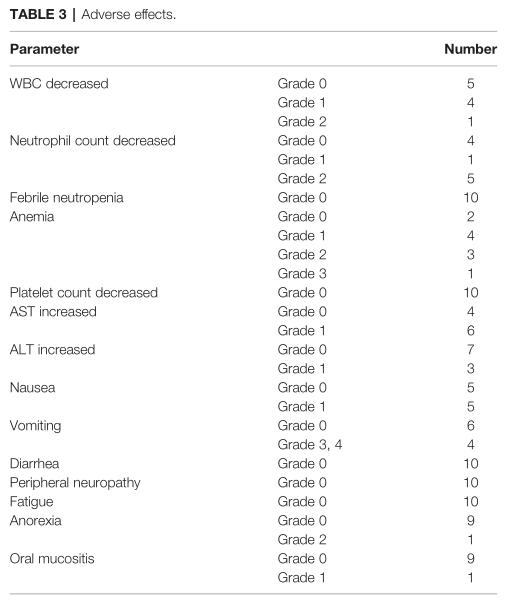
10例患者均行胃癌根治性切除术。其中3例为全胃切除,7例为远端胃切除。术后平均住院时间为9天,5例患者术后出现轻微或中度并发症。无吻合口漏,无再次手术,无手术并发症死亡。
手术并发症
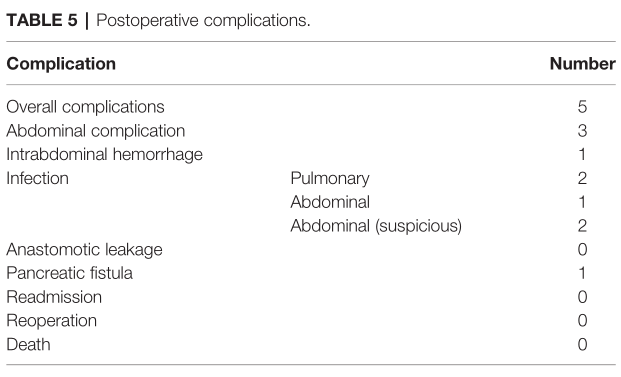
病理报告证实10例患者中有9例实现了R0切除。1例患者切除标本下缘肿瘤阳性,考虑R1切除。中位检查淋巴结数为28个,根据ypTNM分级分为III期8例。1例患者肿瘤完全消退(TRG 1a), 2例患者肿瘤次全消退。
肿瘤病理退缩
9例患者完成了4个周期的术后化疗。1例患者拒绝辅助化疗。只有1例患者完成了全部4个周期足剂量的术后化疗。其他患者的辅助化疗剂量减少25%或更少。
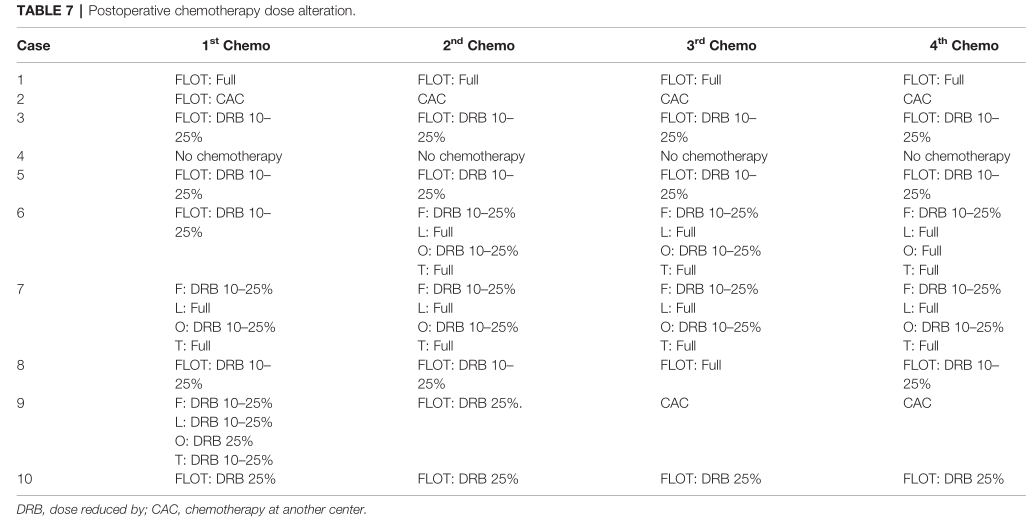
术后辅助化疗
中位随访时间为23.13个月。10例患者均及时随访,8例仍存活;其中7例患者在最后一次随访时(2020年5月14日)没有任何复发迹象。1例患者在第一个化疗周期8个月后腹膜和卵巢转移复发,仍在接受化疗。因此,中位随访时间为23.13个月时,8例患者获得总生存期(OS), 7例患者获得无复发生存期(RFS)。两名患者死亡,其中一人死于腹膜后转移。该患者OS时间为26个月,RFS时间为6个月。另一名患者死于腹膜转移和克鲁肯伯格瘤。该患者的操作系统时间为10.6个月,RFS时间约为6个月。
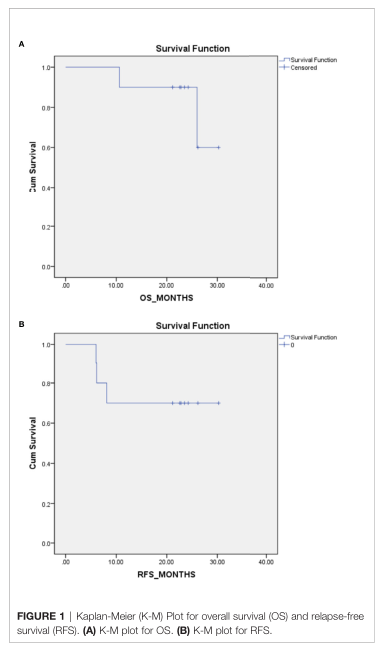
OS
综上,研究表明,FLOT方案作为中国局部晚期胃癌新辅助治疗安全有效,辅助治疗的剂量应适当调整。肿瘤病理退缩以及生存需要进一步大样本队列验证。
原始出处:
Sah BK, Xu W, Zhang B, Zhang H, Yuan F, Li J, Liu W, Yan C, Li C, Yan M, Zhu Z. Feasibility and Safety of Perioperative Chemotherapy With Fluorouracil Plus Leucovorin, Oxaliplatin, and Docetaxel for Locally Advanced Gastric Cancer Patients in China. Front Oncol. 2021 Jan 18;10:567529. doi: 10.3389/fonc.2020.567529. PMID: 33537232; PMCID: PMC7848150.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#局部晚期#
42
#手术期#
40
#可行性#
53
#Oncol#
43
#晚期胃癌#
46
#局部#
24
学习学习
36
不断学习
53