J Clin Endocrinol Metab:特立帕肽后使用地诺单抗治疗绝经前妇女的特发性骨质疏松症
2022-05-09 sunshine MedSci原创
我们既往研究中,研究人员发现特立帕肽与41名患有特发性骨质疏松症(IOP)的绝经前妇女的腰椎(LS)、全髋关节(TH)和股骨颈(FN)的骨矿物质密度(BMD)大幅增加有关,而桡骨远端则有小幅下降。
我们既往研究中,研究人员发现特立帕肽与41名患有特发性骨质疏松症(IOP)的绝经前妇女的腰椎(LS)、全髋关节(TH)和股骨颈(FN)的骨矿物质密度(BMD)大幅增加有关,而桡骨远端则有小幅下降,这些妇女都受到低创伤性骨折和/或极低BMD的严重影响。如果不使用抗骨质疏松剂,特立帕肽的作用就会消失。近日,发表于J Clin Endocrinol Metab的一项预先计划的2B期扩展研究评估了12和24个月的地诺单抗对完成24个月特立帕肽治疗的绝经前IOP妇女的影响。

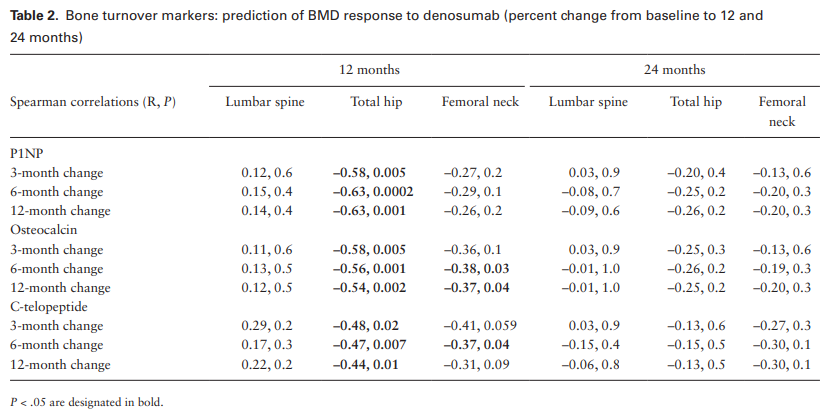
已完成特立帕肽疗程的绝经前女性眼压患者在24个月内每6个月接受一次地诺单抗60mg。主要的结果测量是12个月时LS的BMD的组内变化。次要结果包括其他部位12个月的BMD变化,所有部位24个月的BMD变化,小梁骨评分(TBS),以及骨转换标志物(BTMs)。
结果显示,完成特立帕肽治疗后,32名参与者服用地诺单抗12个月,29名参与者服用地诺单抗24个月,LS(5.2±2.6%和6.9±2.6%)、TH(2.9±2.4%和4.6±2.8%)和FN(3.0±3.8%和4.7±4.9%)处的BMD有统计学意义的增加。在整个24个月的特立帕肽和24个月的地诺单抗治疗期间,LS的BMD增加了21.9±7.8%,TH增加了9.8±4.6%,FN增加了9.5±4.7%(所有P<0.0001)。TBS增加了5.8 ± 5.6%(P < .001)。血清BTM在3个月内下降了75%至85%,并在使用地诺单抗的12个月内保持抑制。地诺单抗的耐受性普遍良好。
综上所述,这些数据支持连续使用特立帕肽和地诺单抗来增加患有严重骨质疏松症的绝经前妇女的BMD。
原始出处:
Elizabeth Shane, et al., Denosumab After Teriparatide in Premenopausal Women With Idiopathic Osteoporosis. J Clin Endocrinol Metab. 2022 Mar 24;107(4):e1528-e1540. doi: 10.1210/clinem/dgab850.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#绝经前#
27
#MET#
32
#Meta#
36
#特发性#
22
#绝经#
33
#特立帕肽#
0
#骨质#
34