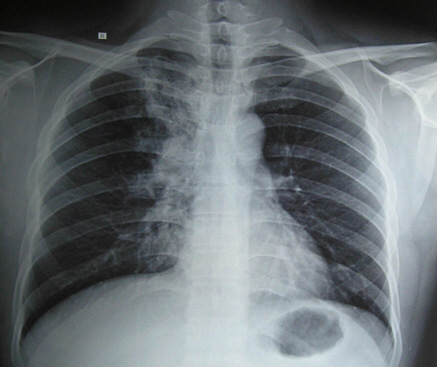
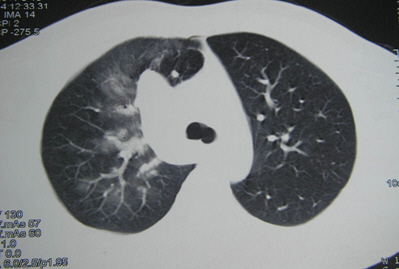
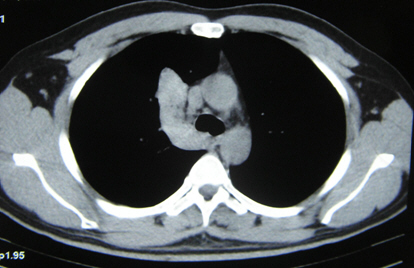
病例:抗结核治疗有效,3年后才发现竟然是误诊!
2018-05-08 王俊,叶龙玲 MedSci原创
肺结核查抗酸杆菌不一定会是阳性,但是当患者症状符合结核特征时,常会尝试进行经验性治疗,若治疗有效则会考虑诊断为肺结核,但是今天的这一例病例却出现了差错,到底是怎么回事呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














学习了,谢谢作者分享!
80
#结核#
24
#抗结核#
41
学习了
70
学习了
0
学习一下谢谢
70
一起学习学习
73