Ann Oncol:二线Osimertinib(奥希替尼)联合贝伐珠单抗并不能明显改善EGFR突变晚期NSCLC获得T790M突变患者的预后
2022-02-09 yd2015 MedSci原创
研究表明,Osimertinib(奥希替尼)联合贝伐珠单抗二线治疗并不能明显改善EGFR突变晚期NSCLC获得T790M突变患者的预后。
Osimertinib(奥希替尼)是治疗EGFR突变NSCLC患者获得T790M突变时的标准二线治疗,其与贝伐珠单抗联合治疗的疗效尚不明确。因此,Annals of Oncology杂志上发表了一项II期研究BOOSTER的成果,评估二线Osimertinib(奥希替尼)联合贝伐珠单抗对比Osimertinib(奥希替尼)单药治疗EGFR T790M突变晚期NSCLC患者的疗效。
BOOSTER研究是一项开放标签、随机II期临床研究。主要研究终点是研究者评估的无进展生存期(PFS)。次要终点为总生存期(OS)、客观缓解率(ORR)和不良事件(AEs)。
在2017年5月至2019年2月期间,155例患者被随机分组(联合组:78例;单药组: 77例)。中位年龄为67岁,大多数为女性(62%)、非亚裔(59%)和从不吸烟者(60%),ECOG=1(64%)。70%患者为IVa期。109例(70%)患者检测到EGFR 19外显子缺失。基线时,14%的患者有脑转移,14%有肝转移,10%有胸腔积液和腹水。有15.5%的患者在随机分组前接受过铂类化疗。
中位随访时间为33.8个月[四分位间距(IQR): 26.5-37.6个月](联合组:32.6个月;单药组:34.5个月)。两组患者的中位PFS无显著差异,联合组为15.4个月(95% CI 9.2-18.0),单药组为12.3个月(95% CI 6.2-17.2)[log-rank P 0.71;HR (95% CI): 0.94(0.66-1.33)]。联合组和单药组的1年PFS率分别为60.3% (48.4%-70.3%) 和50.8% (39.1% -61.5%)。
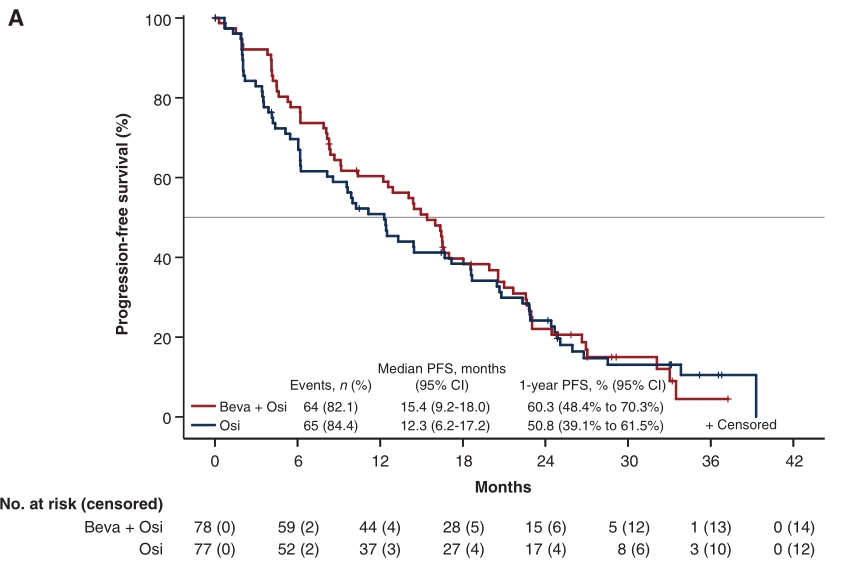
PFS
亚组分析时,联合组可改善目前吸烟者和既往吸烟者的中位PFS [HR: 0.57 (0.33-0.98);Wald检验P=0.043],但不能改善不吸烟患者的PFS (HR: 1.29 (0.82-2.02);Wald检验P=0.28)。
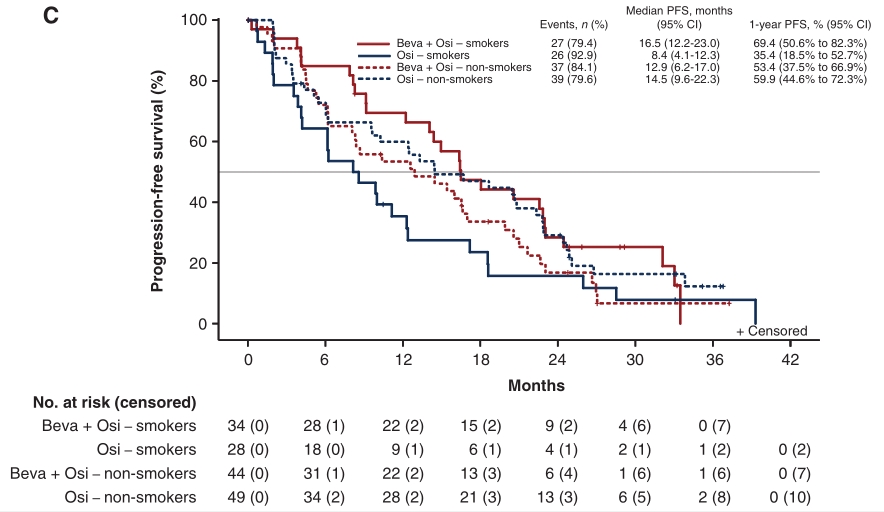
不同吸烟状态治疗PFS差异
联合治疗组的中位OS为24.0个月(95% CI 17.8-32.1),而单药组的中位OS为24.3个月(95% CI 16.9-37.0),OS无显著差异[log-rank P=0.89;HR:1.03 (0.68-1.56)。联合组在数值上延长目前吸烟者和既往吸烟者的中位OS[HR: 0.64 (0.33-1.22); Waldtest P=0.18],同样不能改善不吸烟患者的OS。

OS
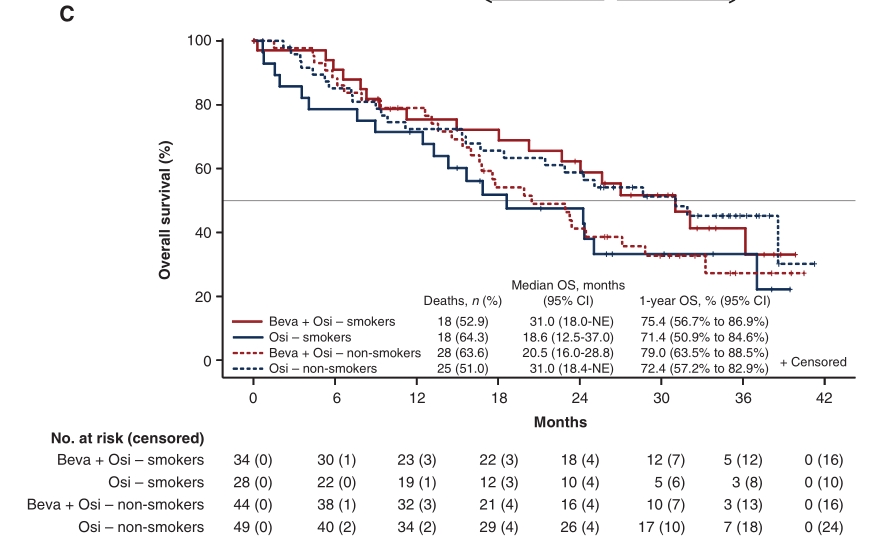
不同吸烟状态治疗OS差异
两治疗组的ORR均为55% (95% CI 43%-66%),联合治疗组和单药治疗组的DCR分别为90% (95% CI 81%-95%)和82% (95% CI 71%-90%)(P=0.17)。
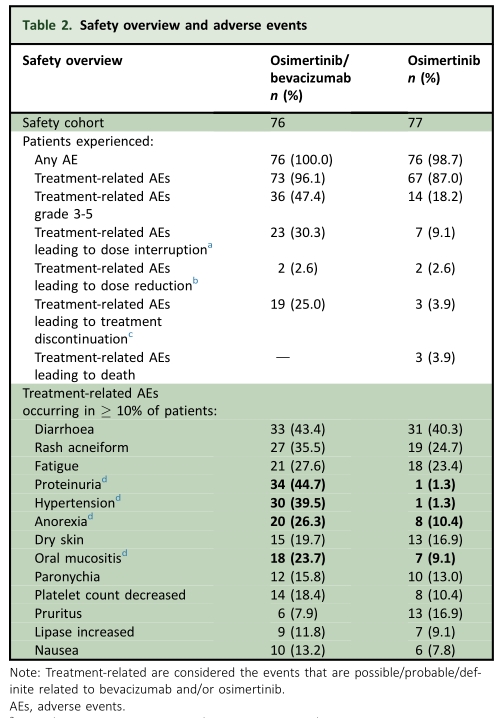
在安全队列中,153例患者中有152例(99%)发生了至少一次任何级别的AE(每组76例)。在联合治疗组和单药治疗组中,发生任何级别TRAE的患者比例分别为96%和87%,而3级TRAE的患者比例分别为47%和18%。
综上,研究表明,Osimertinib(奥希替尼)联合贝伐珠单抗二线治疗并不能明显改善EGFR突变晚期NSCLC获得T790M突变患者的预后。
原始出处:
Soo RA, Han JY, Dafni U, et al. A randomised phase II study of osimertinib and bevacizumab versus osimertinib alone as second-line targeted treatment in advanced NSCLC with confirmed EGFR and acquired T790M mutations: the European Thoracic Oncology Platform (ETOP 10-16) BOOSTER trial. Ann Oncol. 2022 Feb;33(2):181-192. doi: 10.1016/j.annonc.2021.11.010. Epub 2021 Nov 26. PMID: 34839016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#贝伐珠#
38
#T790M#
42
#Oncol#
61
#奥希替尼#联合#贝伐单抗#
100
#晚期NSCLC#
43
#osimertinib#
49
#贝伐#
35
#GFR#
37