Hepatology:华西二院刘聪教授团队揭示乙肝病毒相关肝癌发病机制
2019-03-31 佚名 四川大学华西第二医院
四川大学华西第二医院刘聪教授团队与基础医学院联合多个研究机构,在乙肝病毒(HBV)相关肝癌发病机制方面取得重要进展。
四川大学华西第二医院刘聪教授团队与基础医学院联合多个研究机构,在乙肝病毒(HBV)相关肝癌发病机制方面取得重要进展。相关研究成果以“乙肝病毒编码的X蛋白的抗回切活性”(Theanti-resection activity of the X protein encoded by Hepatitis Virus B)为题,于近日在国际期刊《Hepatology》(《肝病学》、IF14.079)上在线发表。刘聪教授为本文唯一通讯作者,任来峰、曾鸣、唐子执和李明远为共同第一作者。
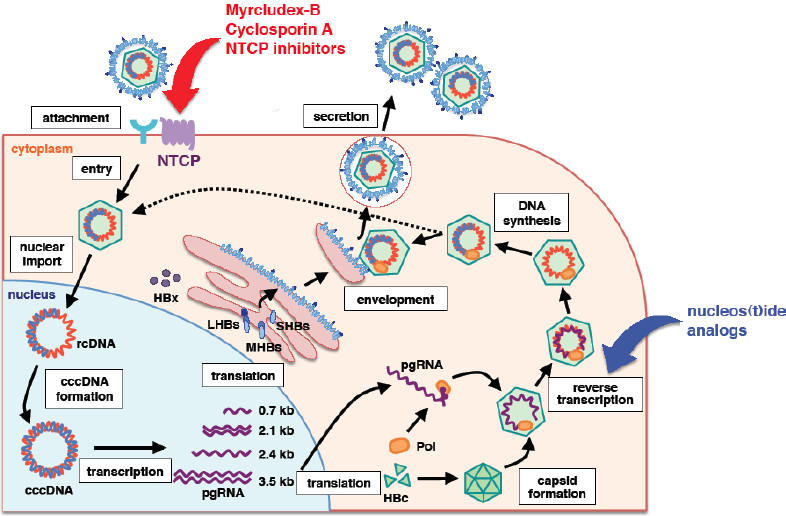
原发性肝癌是我国最为常见的难治性恶性肿瘤之一,HBV感染是其发病的重要风险因素。HBV编码的X蛋白(HBx)不仅对病毒自身复制至关重要,还能干扰宿主细胞基因表达、组蛋白修饰及基因组稳定性等多方面功能,被认为是最主要的病毒癌蛋白之一。然而到目前为止,HBx导致肝癌发生的具体分子机制仍不清楚。
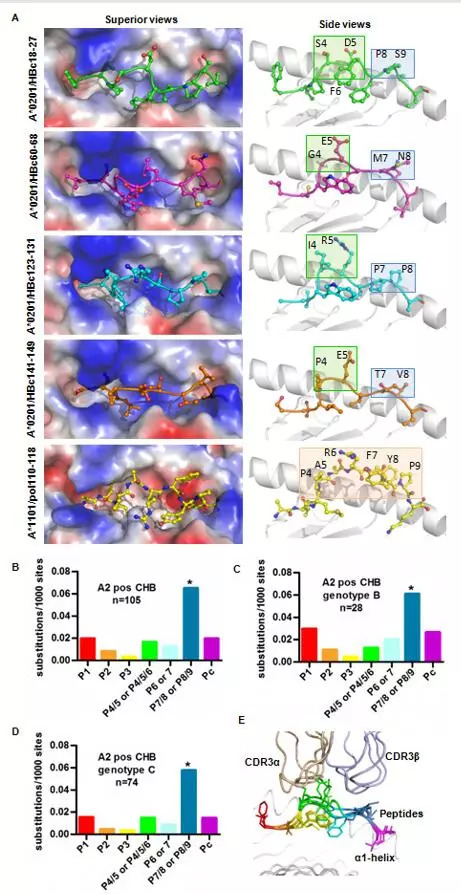
刘聪教授课题组研究发现,在HBV感染或整合病毒基因组的肝细胞中,HBx通过扰乱DNA双链断裂位点的切割处理,引起宿主细胞同源重组修复缺陷。在此基础上,发现HBx通过结合DDB1并扰乱CRL4WDR70泛素酶复合体,抑制组蛋白H2B单泛素化在断点附近的延伸,从而阻断DNA双链断裂的末端回切过程。该研究表明,HBx引起的DNA末端回切与肿瘤发生密切相关,HBV阳性肝癌是一种新的同源重组缺陷型肿瘤,为肝癌的发病机制和治疗提供了新的思路。
同时,该项研究强烈提示了靶向同源重组缺陷型肿瘤的PARP抑制剂具有治疗HBV相关肝癌的潜力,并已在有关肝癌治疗模型中得到初步的验证。有关药物二次应用已经申请了国家发明专利,具有独立知识产权,四川大学华西第二医院与北京大学为共同专利权人。该项工作得到了国家自然科学基金项目(31471276,31771580)的系列资助。
原始出处:Laifeng Ren, Ming Zeng, Zizhi Tang, et al. The anti‐resection activity of the X protein encoded by Hepatitis Virus B. Hepatology. 21 February 2019
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#癌发病#
28
***
66
#EPA#
34
#华西#
33
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
49