Proxalutamide用于治疗美国住院COVID-19患者的III期临床试验,首次对患者给药
2021-10-04 Allan MedSci原创
Kintor Pharma今天宣布,于10月1日进行的Proxalutamide III期临床试验(用于治疗住院COVID-19患者)已在美国招募并给药了第一位患者。
Kintor Pharma今天宣布,于10月1日进行的Proxalutamide III期临床试验(用于治疗住院COVID-19患者)已在美国招募并给药了第一位患者。Proxalutamide是唯一进入III期MRCT临床试验的小分子口服药物,用于治疗住院COVID-19患者。
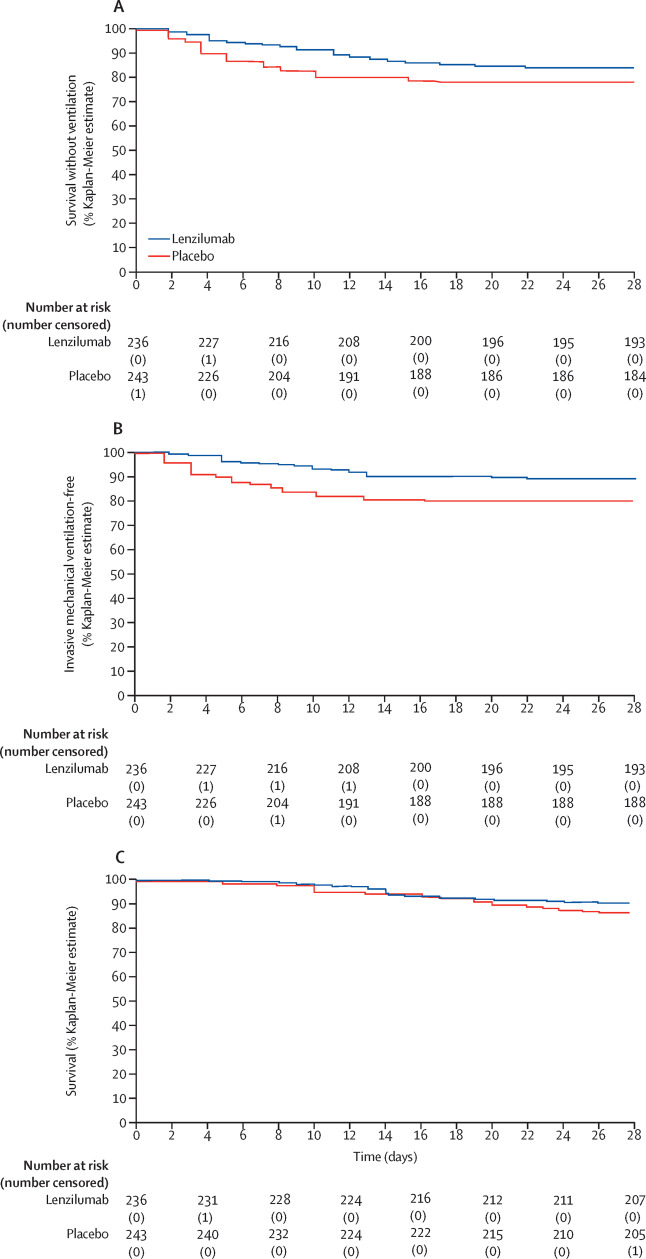
美国III期试验是一项随机、双盲、安慰剂对照、多区域关键性试验,旨在评估proxalutamide在住院 COVID-19患者中的疗效和安全性。试验的主要终点是第30天评估的持续恢复时间,试验的次要终点是30天死亡率。这项关键研究已获得美国FDA、中国CDE、菲律宾FDA和巴西ANVISA的批准,并正在寻求欧洲和亚洲更多监管机构的批准。
Proxalutamide是一种非甾体类抗雄激素(AR)药物,是雄激素受体的选择性高亲和力拮抗剂,正在开发用于COVID-19、前列腺癌和乳腺癌的潜在治疗。Proxalutamide靶向AR-ACE2/TMPRSS2信号轴可以通过转录下调TMRPSS2和ACE2的表达来显著抑制病毒进入宿主细胞。同时,Proxalutamide通过激活Nrf2通路促进病原体清除并减少炎症,该通路激活多种抗氧化基因和蛋白质,并降低细胞因子反应的强度,这可能对COVID-19感染患者具有临床益处。
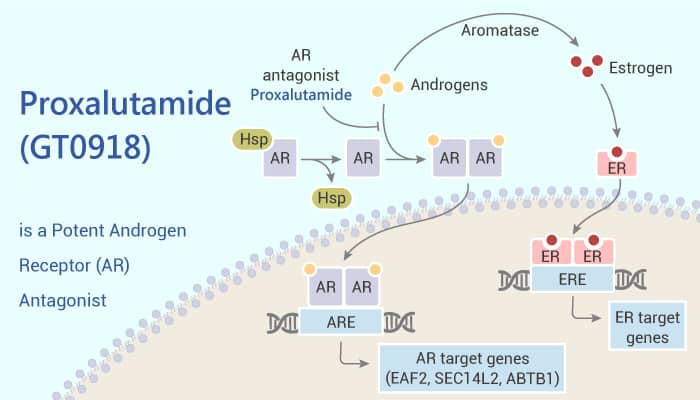
Kintor Pharma创始人、董事长兼首席执行官Youzhi Tong博士评论说:“作为AR拮抗剂,proxalutamide已经展示了明确的作用机制,包括下调ACE-2和 TMPRSS2蛋白,提高NrF-2的表达并抑制IL-6和TNF-α等,从而最大限度地减少细胞因子风暴和组织损伤,这表明proxalutamide可作为治疗重症COVID-19患者的可能方法”。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#III#
33
#I期临床试验#
46
#I期临床#
39
#II期临床试验#
29
#COVID-19患者#
29
#II期临床#
25
#III期临床试验#
52
#III期#
25
#PRO#
16
👍
68