南方医院刘思德团队胶囊内镜项目获中国高校科交会金奖
2017-07-04 佚名 南方医院
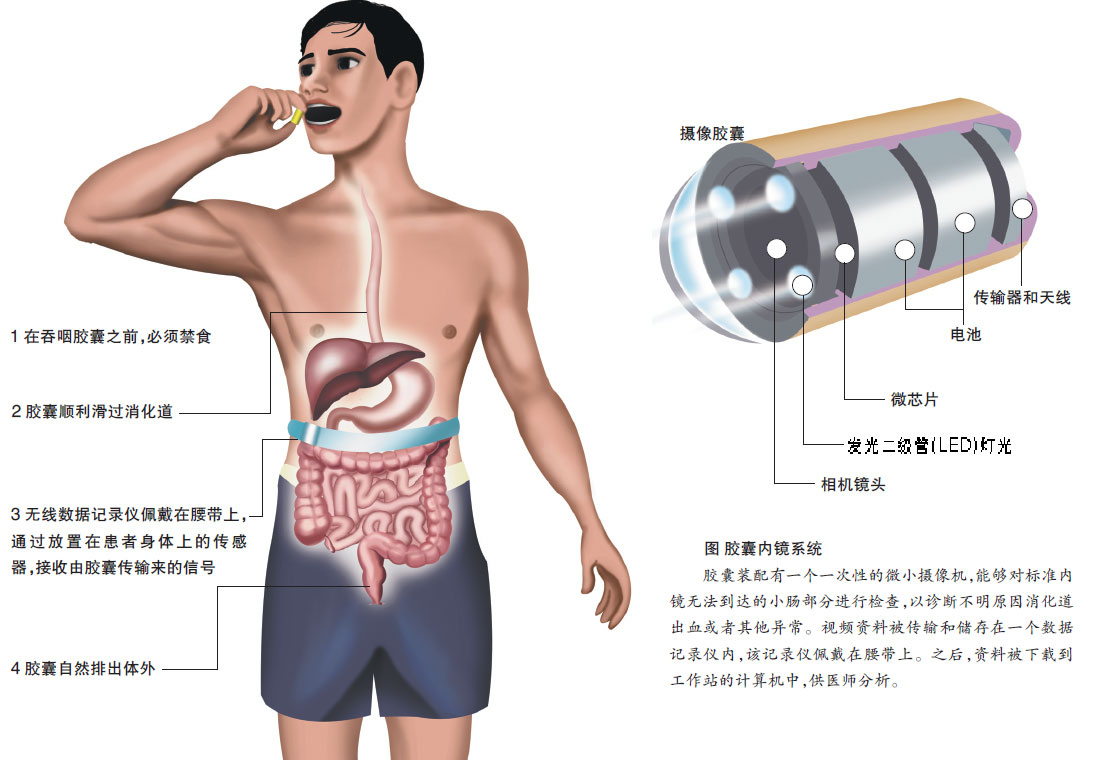
在不久前闭幕的首届中国高校科技成果交易会上,南方医科大学南方医院消化内科主任医师 刘思德团队研发的“智能胶囊胃镜系统”项目得到专业评委、投资商高度认可,从300所海内外高校、约10000项科技项目中脱颖而出,荣获首届中国高校科交会最高奖项特别金奖。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#南方医院#
33
学习了谢谢分享!!
70
学习了,谢谢
76
#内镜#
0
#高校#
34
#胶囊内镜#
41
学习了,谢谢
67
非常好的文章,学习了,很受益
74
谢谢分享受益匪浅
66
赞祝贺祝贺祝贺
31