Lancet Neurology:ORATORIO试验的长期随访:早期和持续ocrelizumab治疗对原发性进行性MS的疾病进展具有益处
2020-12-08 MedSci原创 MedSci原创
多发性硬化症(MS)是一种中枢神经系统慢性自身免疫病,本病以多发病灶、缓解、复发病程为特点,好发于视神经、脊髓和脑干。ocrelizumab是一种B细胞CD20抗原抑制剂单克隆抗体。
多发性硬化症(MS)是一种中枢神经系统慢性自身免疫病,本病以多发病灶、缓解、复发病程为特点,好发于视神经、脊髓和脑干。ocrelizumab是一种B细胞CD20抗原抑制剂单克隆抗体,能有效地控制缓解MS病情。
ORATORIO是一项国际性、多中心、双盲、随机、安慰剂对照的III期试验,它在182个研究地点进行,包括在美洲、澳大利亚、欧洲、以色列、新西兰和俄罗斯等29个国家的学术中心、医院和社区专业中心。入组条件为年龄在18-55岁的原发性进行性MS患者,其残疾状态扩展量表(EDSS)评分为3.0-6.5分。曾经接受过B细胞靶向治疗或其他免疫抑制药物治疗的患者则被排除在外。本研究主要报告了目前正在进行的超过3.5研究年的开放性扩展随访(其中1个研究年定义为48周)的中期安全性和有效性数据。本文专注于临床上有意义的指标--包括行走、上肢功能和需要轮椅的时间以及磁共振成像测量,这些在原发性进行性MS中经常被忽视。
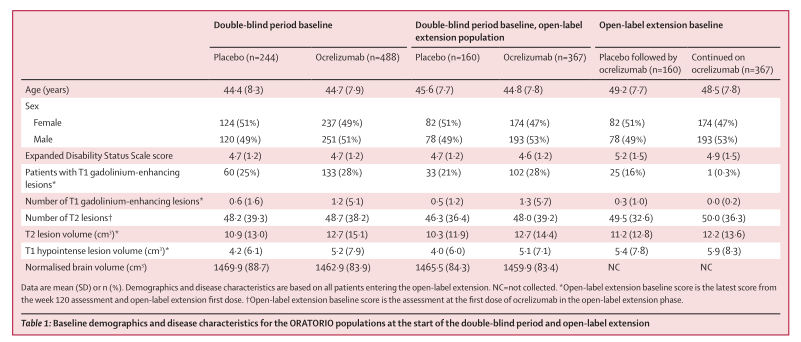
合格的受试者被随机分配(2:1),每24周接受一次600mg的ocrelizumab静脉注射(两次300mg的注射间隔14天)或安慰剂,持续至少120周,直到出现预先指定数量(n=253)的残疾事件。在双盲阶段之后,患者进入了一个持续时间可变的延长控制期。在这段时间之后,患者可以进入一个可选的开放标签延长期,在此期间他们可以继续使用ocrelizumab或从安慰剂切换到ocrelizumab。在24周时,通过四项测量(即EDSS评分增加,增加≥20%完成9-Hole Peg测试[9HPT],增加≥20%进行定时25英尺步行[T25FW],综合进展定义为这三项单独测量中任何一项的首次确认发生),以及需要轮椅的时间(EDSS≥7),并对常规MRI检查结果进行分析。
在至少6.5个研究年(每个研究年度48周)的随访后,在大多数24周确认的残疾进展的测量中,早期开始使用ocrelizumab的患者的残疾测量进展患者比例低于最初接受安慰剂的患者:EDSS,51.7%比64.8%(差异13.1%[95%CI 4.9-21.3];p=0·0018);9HPT,30.6%vs 43.1%(12.5% [4.1-20.9]);p=0·0035);T25FW,63.2%对70.7%(7.5%[-0.3至15.2];p=0·058);复合进展,73.2%vs 83.3%(10.1%[3.6-16.6];p=0·0023和确定需要轮椅的时间,11.5%对18.9%(7.4%[0.8-13.9];p=0.0274)。在研究结束时,在T2损伤体积(0.45%vs 13.00%,p<0.0001)和T1低信号损伤体积(36.68%对60.93%,p<0.0001)方面,早期开始使用Oclizumab的患者的基线变化百分比低于安慰剂组。
综上所述,根据几项结果指标的评估,ORATORIO研究中6.5个研究年随访研究的数据显示早期和持续ocrelizumab治疗对原发性进行性MS的疾病进展具有一致和持续的益处。此外,ocrelizumab在该患者组6.5个研究年的安全性令人放心,并与复发多发性硬化症的相似长期数据一致。
Wolinsky, Jerry S et al. Long-term follow-up from the ORATORIO trial of ocrelizumab for primary progressive multiple sclerosis: a post-hoc analysis from the ongoing open-label extension of the randomised, placebo-controlled, phase 3 trial. The Lancet Neurology, Volume 19, Issue 12, 998 - 1009
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病进展#
41
#进行性#
32
#mAb#
43
#Neurol#
32
#长期随访#
40
#Lancet#
42
早期和持续ocrelizumab治疗对原发性进行性MS的疾病进展具有一致和持续的益处
76
#原发性#
41
#Ocrelizumab#
37
#CRE#
46