JNCCN:乳腺癌患者CDK4/6抑制剂哌柏西利进展后使用阿贝西利治疗的疗效:多中心临床经验
2021-05-11 yd2015 MedSci原创
乳腺癌患者CDK4/6抑制剂哌柏西利进展后使用阿贝西利治疗仍有临床获益
细胞周期蛋白依赖性激酶4和6抑制剂(CDK4/6抑制剂)联合内分泌治疗目前已经成为激素受体阳性转移性乳腺癌(HR+MBC)一线治疗或内分泌治疗进展后的标准方案。目前研究证实三种CDK4/6抑制剂药物(哌柏西利、阿贝西利、ribociclib)联合内分泌治疗均可改善HR+/HER2- MBC的无进展生存期(PFS)。II期MONARCH-1临床试验证实了阿贝西利单药治疗内分泌或化疗进展的HR+MBC疗效(PFS 6.0个月,95% CI, 4.2–7.5个月)。但是该试验没有纳入哌柏西利治疗进展的患者。目前临床上有部分医师借鉴HER2阳性乳腺癌患者曲妥珠单抗失败后继续抗HER2治疗的经验,CDK4/6抑制剂治疗一线或二线治疗的HR+转移性乳腺癌,继续实施其他CDK4/6抑制剂治疗。但是,目前没有研究评估一线应用哌柏西利失败后应用阿贝西利的疗效。
因此,国外学者在Journal of The National Comprehensive Cancer Network(JNCCN)杂志上发表了相关研究,主要研究CDK4/6抑制剂哌柏西利进展后使用阿贝西利治疗的疗效。

该研究为多中心回顾性研究,主要纳入美国6个癌症中心的87例HR+MBC患者,所有患者一线治疗应用的都是哌柏西利。符合条件患者回顾性收集相关临床指标,包括初始癌症诊断时的年龄、转移性诊断和死亡或最近的临床就诊日期等。
研究数据表明,在入组的87例患者中,阿贝西利治疗患者的中位无进展生存期(PFS)为5.3个月(95% CI, 3.5–7.8个月),中位总生存期(OS)为17.2个月(95% CI, 13.2个月–未达到)。与MONARCH-1试验相似(PFS 6.0个月,95% CI, 4.2–7.5个月)。

患者的PFS 和OS
患者CDK4/6抑制剂哌柏西利治疗失败后,80.5%患者接受了阿贝西利联合治疗,联合内分泌治疗中有47.1%患者使用了氟维司群,27.6%患者使用了芳香化酶抑制剂,5.8%患者使用了他莫昔芬和其他,19.5%患者接受了阿贝西利单药治疗。
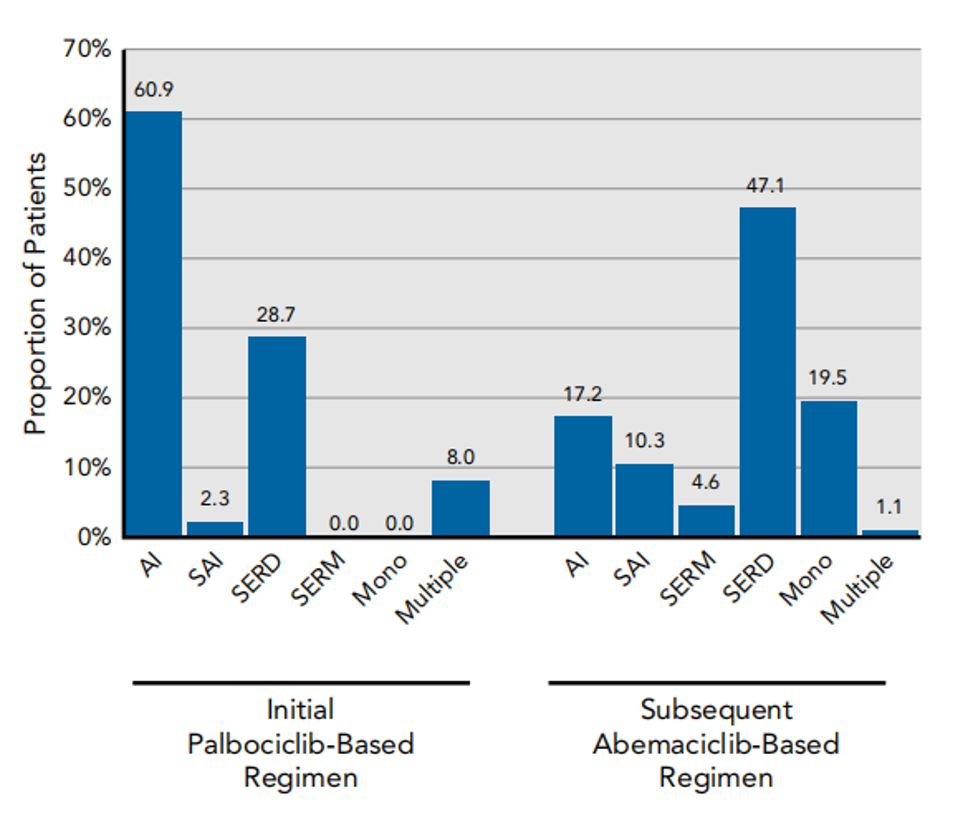
后续阿贝西利用药情况
接着研究表明,哌柏西利为基础的治疗持续时间与后续阿贝西利治疗的持续时间无明显相关。
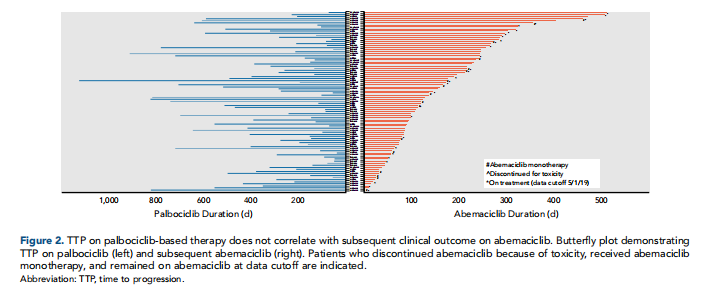
两者治疗持续时间无明显相关
接受阿贝西利治疗患者的耐受性良好,只有少数患者(9.2%)因不良反应而停用,但疾病未发生进展。停药原因包括转氨酶升高/肝损伤、腹泻、恶心/呕吐和虚弱。 贫血是最常见的不良事件(任何级别:72.4%;3~4级:14.9%)。中性粒细胞减少(任何级别:63.2%;3~4级:12.6%)和血小板减少症(任何级别:46.0%;3~4级:9.2%)也很常见。
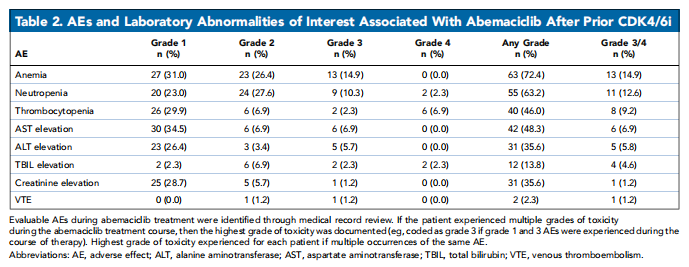
治疗相关不良事件
研究者也尝试使用二代测序(NGS)寻找耐药的预测标志物,研究表明可能与RB1、ERBB2和CCNE1相关因子的改变有关。
综上,乳腺癌患者CDK4/6抑制剂哌柏西利进展后使用阿贝西利治疗仍有临床获益。
原始出处:
Seth A. Wander, Hyo S. Han, Mark L. Zangardi, et al. Clinical Outcomes With Abemaciclib After Prior CDK4/6 Inhibitor Progression in Breast Cancer: A Multicenter Experience.Journal of The National Comprehensive Cancer Network.2021. DOI: https://doi.org/10.6004/jnccn.2020.7662
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床经验#
54
#CDK4#
35
#抑制剂#
31
#多中心#
37
#NCCN#
37
#CDK#
35
#CDK4/6#
34
#乳腺癌患者#
25
谢谢梅斯提供这么好的信息,学到很多
45