Alzheimer Dementia :路易体痴呆患者,核心特征如何随时间变化
2021-12-09 Freeman MedSci原创
男性、RBD和无新皮层缠结的路易体病与可能的DLB的较早潜伏期有关。
路易体痴呆(DLB)是一种进行性的神经退行性疾病,其特点是认知障碍和四个核心特征的不同组合,包括快速眼动睡眠行为障碍(RBD)、帕金森症、认知波动和完全形成的视觉幻觉(VH)。
DLB的病理标志是与路易相关的病理,但在尸检样本中至少有一半的DLB患者同时存在不同程度的阿尔茨海默病(AD)相关病理。 尽管人们对DLB有了更多的认识,也有了结构化的诊断工具,但DLB的诊断灵敏度已提高到85%,尽管对没有新皮层神经纤维缠结的路易体病来说灵敏度较高,而对有广泛的新皮层缠结者来说灵敏度较低。
确立临床上可能的DLB诊断需要两个或更多的核心特征,并取决于每个核心特征何时宣称自己。在临床上,男性更有可能有RBD的报告史,和无新皮质缠结的路易体病。然而,并非所有DLB患者都会出现RBD,混合病理的患者RBD的比率较低,从认知开始到DLB诊断的延迟时间较长。
藉此, 梅奥诊所的Parichita Choudhur等 探究了男性和女性可能患DLB的核心特征的时间顺序,并探究在临床队列和尸检子集中,性别、RBD状态和病理学是否与较早或较晚诊断为可能的DLB有关。
在488名可能的DLB患者中,他们确定了男性和女性以及一个病理亚组(n = 209)的每个核心特征的发病和诊断时间。
他们发现;男性和女性的快速眼动睡眠行为障碍(RBD)在其他核心特征之前发病。男性更有可能出现RBD,并且比女性更早被诊断为可能的DLB。
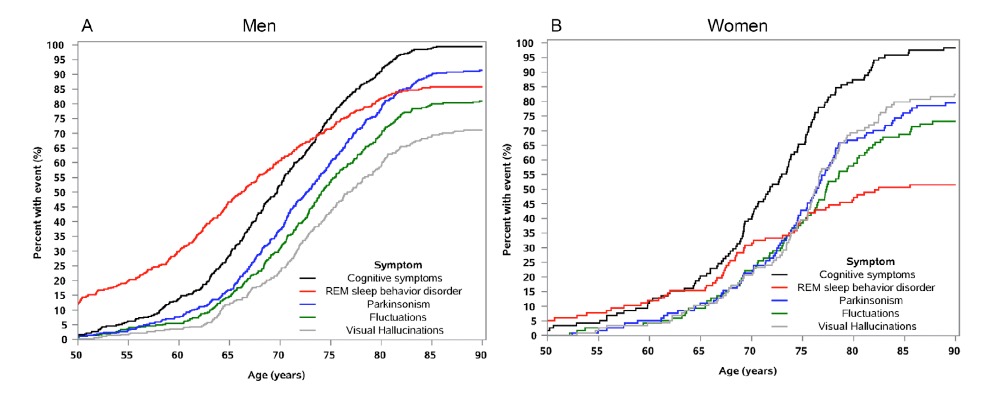
男性的视幻觉是在其他核心特征之后出现的,但在女性,视幻觉出现得更早,并与波动和帕金森症同时出现。
女性在首次就诊时年龄更大,认知能力更差,不太可能有RBD,更可能比男性更晚被诊断为可能的DLB,而且更可能有新皮质缠结。
该研究的重要意义在于发现了:男性、RBD和无新皮层缠结的路易体病与可能的DLB的较早潜伏期有关。
原文出处:
Choudhury P, Graff‐Radford J, Aakre JA, et al. The temporal onset of the core features in dementia with Lewy bodies. Alzheimer’s & Dementia. Published online November 11, 2021:alz.12411. doi:10.1002/alz.12411
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#痴呆患者#
53
#路易体#
40
#dementia#
40
学习学习
64
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
38